Thyroid Health, Weight Loss, and the Power of Carbs
Introduction: Why Thyroid Health Matters
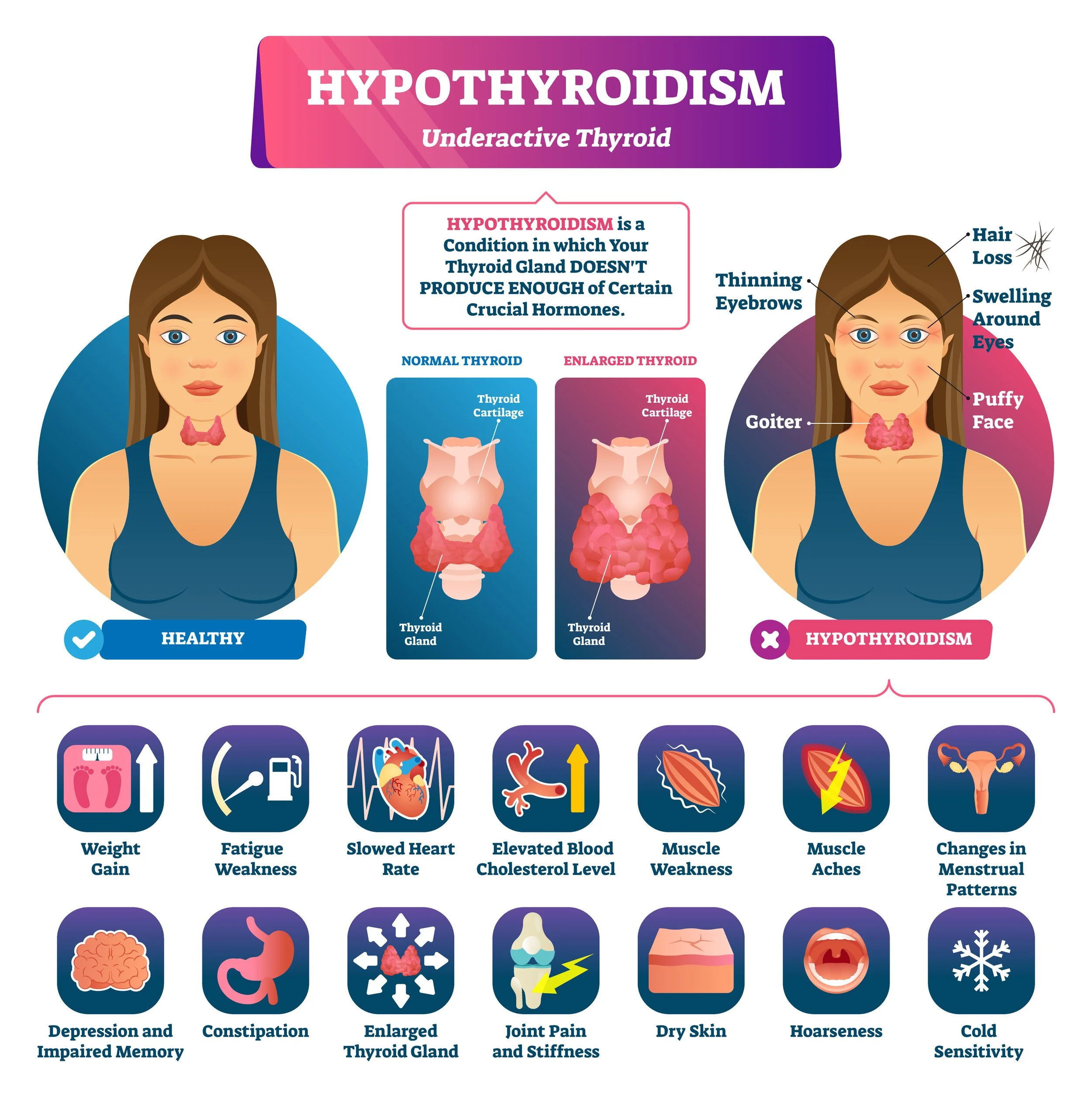
Most people think of thyroid dysfunction as a niche medical issue. In reality, your thyroid is the master regulator of energy. When it slows, every system in your body slows with it — digestion, mood, fertility, fat loss, and even your ability to feel warm.
Unfortunately, modern medicine often overlooks the full scope of hypothyroidism because it relies too heavily on blood tests like TSH. These markers miss what’s happening at the cellular level, where T3 — the active thyroid hormone — determines whether your cells make ATP (energy) or limp along half-starved.
How the Thyroid Works: TSH → T4 → T3 → rT3
The thyroid system runs on a conversion pathway:
TSH (Thyroid Stimulating Hormone): Produced by the pituitary, it tells the thyroid gland to release hormones. Think of TSH as mailing a letter.
T4 (Thyroxine): The storage form, released in larger amounts but biologically inactive. This is the letter arriving in the mailbox.
T3 (Triiodothyronine): The active form, converted from T4, drives cellular energy production. This is the letter getting opened and read.
rT3 (Reverse T3): A “dead-end” hormone made from T4 under stress, starvation, inflammation, or toxin load. This is the letter being returned to sender, clogging up the mail system.
When you’re under stress, cutting calories, or eating low-carb, conversion skews toward rT3. Labs may look “normal” (TSH and T4 in range) while you remain cold, tired, and unable to lose weight — the classic picture of functional hypothyroidism.
The Three Types of Hypothyroidism
Functional Hypothyroidism – driven by stress, low calories, low carbs, toxins, or high rT3. Reversible with lifestyle, nutrition, and sometimes T3 support.
Autoimmune Hypothyroidism (Hashimoto’s) – caused by immune attack on the thyroid gland. Often linked to viral triggers, gut dysfunction, mold, and environmental toxins.
Nutrient-Deficiency Hypothyroidism – caused by lack of cofactors like iodine, selenium, iron, copper, or B vitamins that are necessary for thyroid hormone synthesis and conversion.
Understanding which type (or combination) you’re dealing with is critical for treatment.
Food First: Carbs, Calories, and Detoxification
The thyroid can’t function without fuel. Restricting calories or carbs is one of the fastest ways to suppress T3. Research shows that carbohydrate deprivation directly inhibits the conversion of T4 to T3, leaving you with “normal” bloodwork but classic hypothyroid symptoms — fatigue, hair loss, depression, constipation, cold hands and feet.
Long-term, the best path to thyroid restoration is:
Adequate calories (at least 43–48 kcal/kg lean body mass for recovery).
High carbohydrates (fruit, juice, honey, tubers) to maintain glycogen and conversion to T3.
Low PUFA (polyunsaturated fats) to reduce thyroid-blocking effects at the cellular level.
Detox pathways – supporting the liver to clear excess estrogen, endotoxin, and heavy metals that impair thyroid conversion.
Body Temperature and Pulse as Markers
Body temperature and pulse are simple at-home measures of thyroid status. Ideally:
Waking temp: ~97.8°F
Post-breakfast temp: ~98.6°F
Resting pulse: 75–85 BPM
If temps drop after eating, stress hormones (like cortisol and adrenaline) are running the show, not thyroid.
NDT vs. T3: Why Medication Matters
Historically, Natural Desiccated Thyroid (NDT) was the treatment of choice. It contains both T4 (the pro-hormone) and T3 (the active hormone). For many, NDT restores warmth, energy, and weight regulation.
But in others, the T4 portion fails to properly convert to T3, especially under stress, low-carb dieting, or liver burden. That’s when people experience the classic “NDT stopped working for me” story.
In those cases, small, frequent doses of T3-only (like Cynomel) can be more effective. T3 bypasses the conversion bottleneck and directly fuels the cell. The key is microdosing with meals, not blasting the system with one big dose.
Some people do best with a combination of NDT and added T3, ensuring both storage hormone (T4) and active hormone (T3) are available. Others thrive on T3-only protocols, especially when conversion is chronically impaired. The right approach depends on labs, body temperature, pulse, and symptoms — not TSH alone.
Fat Intake and Our Ancestors
Another overlooked piece is fat intake. Modern Western diets often hover at 35–40% fat, with much of it from unstable seed oils. Historically, many traditional diets hovered closer to 10–15% fat. Excess dietary fat — especially polyunsaturated fats — interferes with thyroid hormone transport into cells and slows metabolism.
The Inuit are often cited as thriving on high-fat diets, but history tells a different story. For much of the year, their fertility rates were very low. Births only increased during the short season when they consumed fresh animal thyroid glands, boosting thyroid function. Without carbs or thyroid tissue, their metabolism and reproduction suffered.
In other words: fat alone didn’t sustain them. Thyroid did.
Weight Loss Through a Thyroid Lens
For those struggling with weight loss, thyroid optimization is not optional. You can slash calories and lose weight, but if thyroid function is low, you’ll mostly burn through muscle and stress hormones, not fat. True fat loss comes when metabolism is high enough that your body feels safe to burn stored energy.
That means:
Enough carbs to keep glycogen full.
Adequate calories (at least 43–48 kcal/kg lean body mass for recovery).
Low PUFA, moderate protein, and modest fat (10–20%) to reduce metabolic drag.
Thyroid support (NDT, T3, or both) if labs, temps, and symptoms show you’re running cold.
Closing Thoughts
Hypothyroidism isn’t just about a sluggish thyroid gland. It’s a systemic problem of low energy production. Starving yourself of carbs, overloading fat, or leaning too hard on T4-only medication all drive the same outcome: cold, tired, infertile, overweight, and stuck.
NDT and T3 supplementation can be powerful tools, but they are best seen as temporary supports. These medications are not foreign chemicals — they are identical to the hormones your body is supposed to make. When stress, poor diet, toxins, or years of under-eating have reduced your own production and conversion, supplementing provides what’s missing so your cells can actually make energy. While you rebuild metabolism with adequate calories, high carbs, low PUFA, and detoxification, thyroid meds help keep your body warm and energized enough to burn fat instead of leaning on stress hormones. Once metabolism is restored, many people can taper off medication and rely on food, lifestyle, and nutrient sufficiency for long-term thyroid health.
References
https://academic.oup.com/edrv/advance-article/doi/10.1210/endrev/bnaf015
https://www.nature.com/articles/s41598-019-41997-2
https://restorativemedicine.org/journal/peripheral-thyroid-hormone-conversion-and-its-impact-on-tsh-and-metabolic-activity/
https://pubmed.ncbi.nlm.nih.gov/1249190/
https://pubmed.ncbi.nlm.nih.gov/11167929/
https://pmc.ncbi.nlm.nih.gov/articles/PMC11314468/
https://pmc.ncbi.nlm.nih.gov/articles/PMC5793233/
https://pubmed.ncbi.nlm.nih.gov/30020/
https://pmc.ncbi.nlm.nih.gov/articles/PMC4044302/
https://pubmed.ncbi.nlm.nih.gov/11167929/
https://pmc.ncbi.nlm.nih.gov/articles/PMC4044302/
https://www.thyroid.org/patient-thyroid-information/ct-for-patients/vol-6-issue-8/vol-6-issue-8-p-3/
https://bmcendocrdisord.biomedcentral.com/articles/10.1186/s12902-024-01612-6