The Hidden Metabolic Dangers of GLP-1 Drugs — And the Better Way Out
There is a better way to lose weight than starving your body and slowing your metabolism.
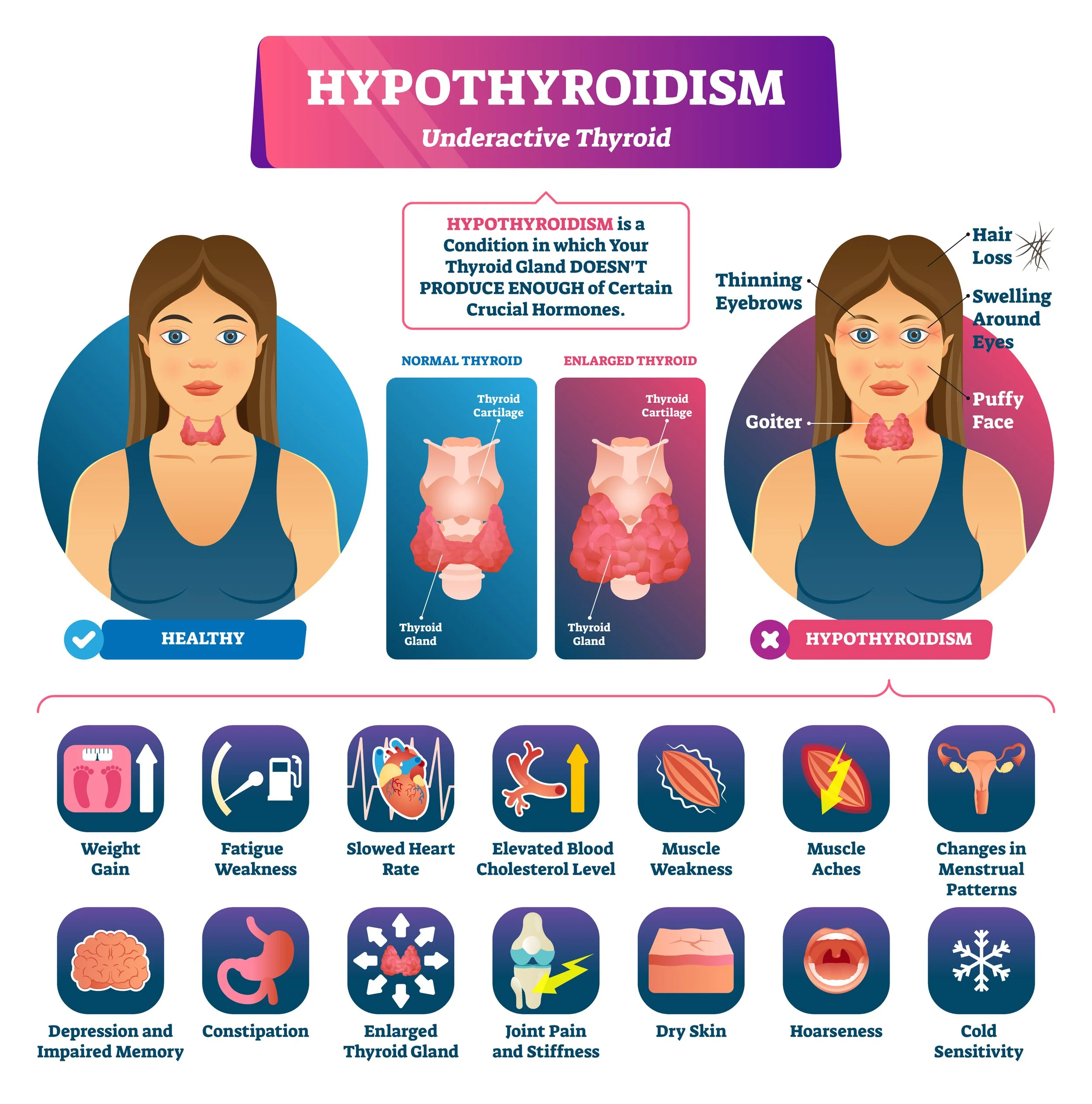
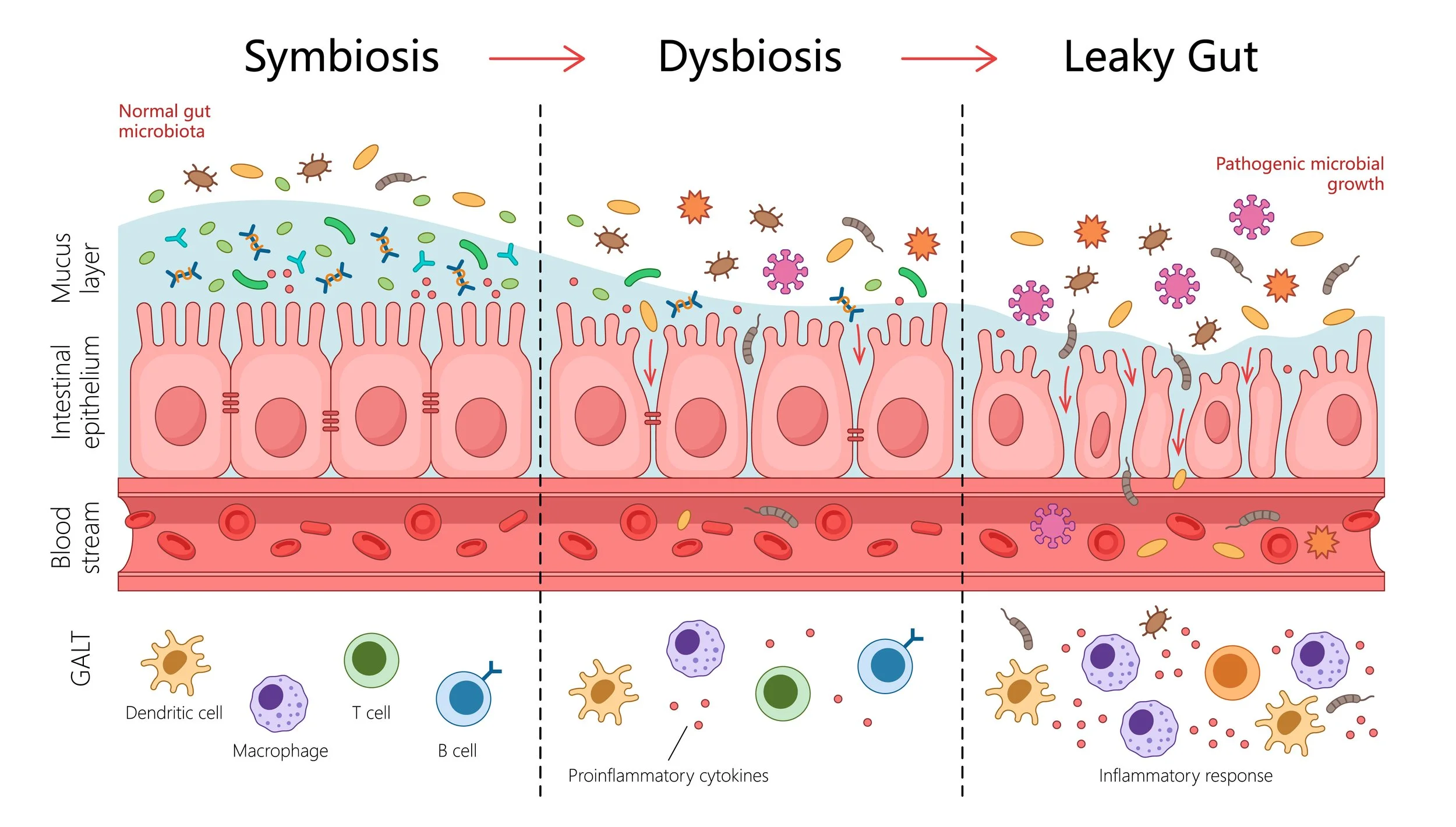
Ozempic, Wegovy, and other GLP-1 medications have exploded in popularity because they promise something that feels almost magical: quick, effortless weight loss without needing to think about food. For someone who has struggled with cravings, slow weight loss, or metabolic frustration, it can feel like the breakthrough they’ve been waiting for. But beneath the surface, these drugs do not address the real reason weight gain happened in the first place. They suppress appetite rather than restoring metabolic function, digestion, thyroid health, or hormonal balance. The deeper issue is not excessive eating; it is insufficient metabolism. Most Americans have a damaged metabolism from seed oils (which are machinery lubricant and currently make up 20% of the American diet), and are running on low thyroid output, sluggish digestion, chronically low energy availability, and diets far too high in fat for their physiology to handle. When metabolism slows, the body stores energy rather than burns it, and weight gain becomes almost effortless.
GLP-1 Drugs Slow Metabolism Rather Than Repairing It
The core problem with GLP-1 drugs is not that they cause weight loss, but how they cause it. They work by shutting down appetite so strongly that many people unintentionally eat far below what the body needs to function. This level of under-eating mimics clinical starvation, and the body responds the way it always does under starvation conditions. Thyroid hormone production drops, body temperature falls, digestion slows, bile thickens, and the detoxification of estrogen and other metabolites becomes impaired. Cortisol rises to compensate for the lack of available fuel, and muscle tissue is broken down for energy. Nothing about this state reflects healing. It reflects conservation and survival.
Most Americans Gain Weight Because Their Metabolism Is Slow, Not Because They Overeat
The cultural message that “people are overweight because they eat too much” is misleading and incomplete. In reality, many Americans consume far more dietary fat than their metabolism is equipped to handle. High-fat intake slows digestion, suppresses mitochondrial efficiency, reduces glucose uptake, and interferes with T4-to-T3 thyroid conversion. Over time, this combination leads to digestive stagnation, low body temperature, hormonal imbalances, and impaired metabolic flexibility. These are the hallmarks of a slow, cold metabolism. Once someone is in this state, weight gain can occur even when calorie intake is not excessive. The body simply does not burn fuel well, and the fuel it cannot burn is stored.
GLP-1 drugs push people deeper into this suppressed metabolic condition. They do not fix the slow thyroid function, sluggish digestion, or impaired carbohydrate metabolism that caused the problem. They amplify it by further reducing caloric intake and slowing gastric emptying even more. The result is a metabolism that becomes increasingly fragile.
Why Rebound Weight Gain Happens After Stopping GLP-1 Drugs
When someone stops taking a GLP-1 medication, appetite returns quickly because the body is trying to correct a prolonged energy deficit. But the metabolic rate does not rebound nearly as fast. Thyroid output remains low, digestion remains slow, muscle mass has often been lost, and cortisol remains elevated. The body begins storing calories rapidly because it has been trained for months to conserve energy. This is why nearly everyone regains weight after stopping these medications, and why many regain more than they lost. This outcome is not a personal failure. It is the natural physiological response to prolonged metabolic suppression.
The Hopeful Truth: Metabolism Can Be Rebuilt
The good news is that the problems that cause weight gain are fixable, and far more fixable than most people realize. A slow metabolism can be restored. A sluggish thyroid can be supported. Digestion can be repaired. Muscle can be rebuilt. Temperature can rise. Energy can return. Appetite can normalize. When the body is given the right support, it becomes naturally inclined toward fat loss because it begins to burn rather than store.
Raising metabolism begins by improving thyroid function — often with natural desiccated thyroid or carefully dosed combinations of T3 and T4 to restore normal hormone signaling. As thyroid function improves, body temperature rises, cellular energy increases, bile becomes thinner, digestion speeds up, and estrogen detoxification becomes more efficient. These changes often happen quickly and can feel dramatic. People notice warmer hands and feet, more stable moods, better digestion, and a return of natural hunger cues that align with stable blood sugar rather than cravings. Side-note: Just because you doctor told you your thyroid is “fine” doesn’t mean that it is, chronically low metabolism lowers Free T3 (active thyroid hormone) and modern medicine only tests TSH and only prescribes T4 medications like Synthroid - which does not fix the problem or tell you how well your thyroid is functioning. Most Americans are hypothyroid and have body tempertures lower than 98.6 in the morning and free T3 below 3.4 from depressed metabolism.
Understanding Energy Availability: The Scientific Foundation of a Fast Metabolism
A core part of restoring metabolism is understanding energy availability, or EA, which measures how much usable energy remains for thyroid function, hormone production, digestion, and cellular repair after accounting for movement. The research here is remarkably consistent: humans require at least 43 calories per kilogram of lean body mass to sustain a healthy metabolic rate. When energy intake falls below this threshold, the body automatically begins shutting down nonessential functions to conserve fuel. Thyroid conversion drops, body temperature decreases, digestion slows, and cortisol rises — all of which make fat loss nearly impossible. To calculate your personal minimum EA, you simply take your lean body mass in kilograms and multiply by 43. For many women, this places true metabolic maintenance between 1,900 and 2,400 calories per day, often significantly higher than what they’ve been eating for years.
Meeting this requirement is not about overeating; it is about eating in the right balance. A simple and reliable template is to aim for one gram of protein per pound of lean body mass, which supports muscle, thyroid function, and metabolic stability. Dietary fat should generally sit around 0.8 grams per pound of lean mass or lower (some people do ok on more), because lowering fat is the safest, most reliable way to increase calories without gaining body fat. When fat is reduced first — especially when seed oils, fried foods, nut milks, nut butters, and processed fats are removed — the body becomes dramatically more efficient at oxidizing carbohydrates. Eating real, whole foods and avoiding industrial seed oils improves insulin sensitivity, enhances bile flow, and prevents the “calorie spillover” that causes fat storage. With protein and fat appropriately set, the remainder of calories should come from carbohydrates. Carbs are indispensable for restoring T3 production, improving digestive motility, raising body temperature, and supporting progesterone and thyroid hormone activity. When EA rises to physiologic levels and the macronutrient distribution is aligned with human metabolism, the entire hormonal system shifts out of famine mode and back into a warm, fat-burning, high-energy state — often with noticeably improved digestion, steadier moods, better sleep, and a renewed sense of vitality.
After a period of restoration in full EA, it is safe to do short, strategic fat-loss periods (I usually recommend 2 weeks at a time) to drop body fat and retain muscle mass. In the body building world, this is called a “cut” and is done in a way that keeps protein and carbs as high as possible to protect the metabolism and thyroid. The literature is very clear that reduces calories for a long period of time - a standard diet, or what occurs on GLP-1 medications - is a starvation state and is extremely hard on the body. It reduces metabolism, impairs hormone health, leads to insomnia and high cortisol, creates depression and anxiety, causes gut problems and slow digestion, and lowers body temperature.
Lowering Dietary Fat and Learning to Burn Carbohydrates Is Essential
Another essential piece of metabolic rehabilitation is reshaping the macronutrient profile away from excessive fat and toward carbohydrates that the body can burn efficiently. Carbohydrates support thyroid conversion, improve mitochondrial function, stabilize blood sugar, increase progesterone, and elevate metabolic rate. When dietary fat is lowered to metabolically appropriate levels, digestion improves, bile flows freely, and the cells regain the ability to oxidize glucose. Many people discover that they were never “carb intolerant.” They were simply eating far too much fat and poisoned by seed oils, which blocked their ability to burn carbohydrates properly. Once this metabolic traffic jam is removed, weight loss becomes much easier.
Restoring Digestion and Motility Is a Cornerstone of Long-Term Fat Loss
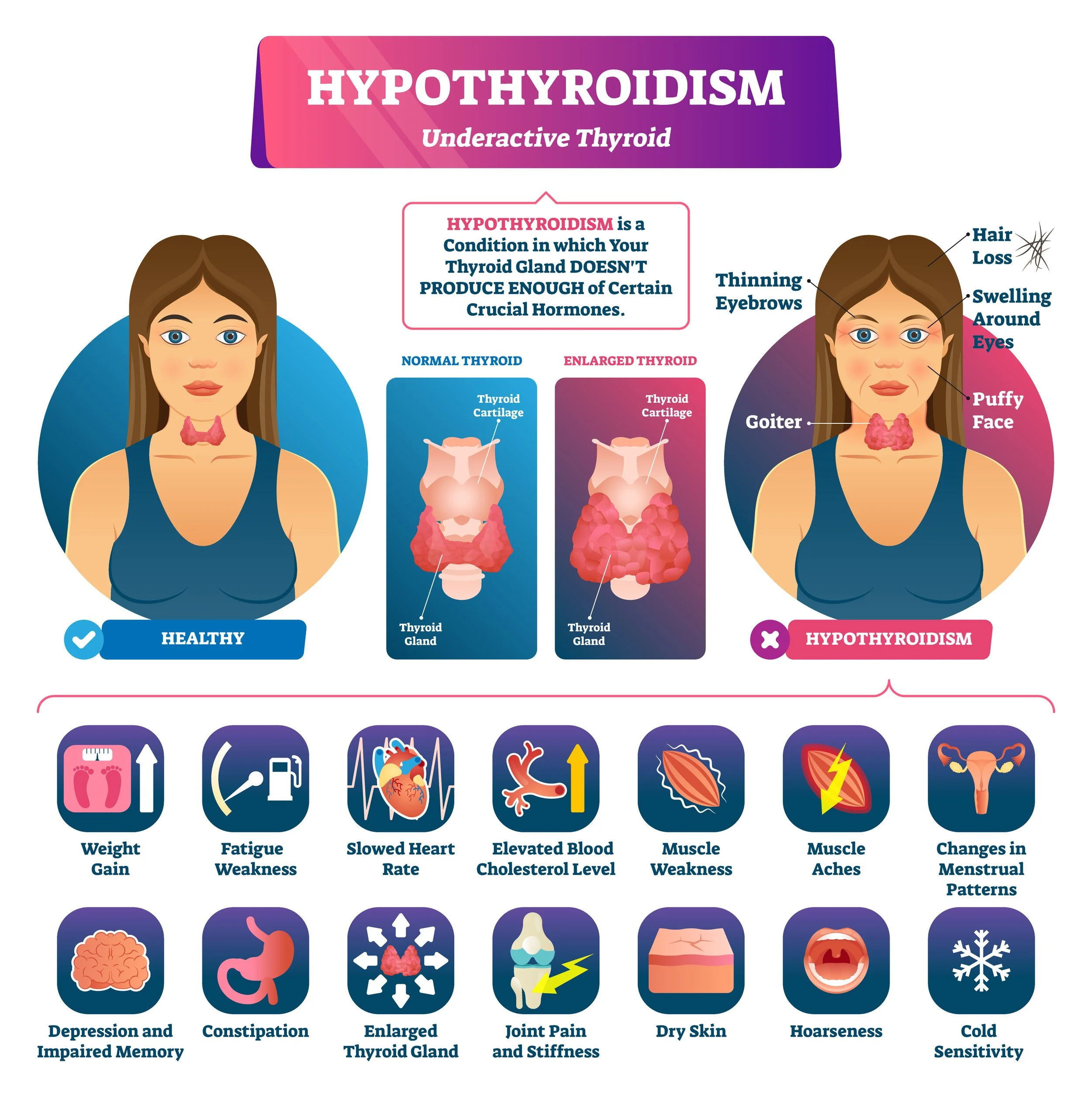
Improving digestion is another central pillar of restoring a fast metabolism. When motility increases, stomach acid and enzymes rise, bile circulates properly, and nutrients can finally be absorbed. This leads to improved hormonal function and more stable energy. It also reduces estrogen recirculation, a major contributor to weight gain, PMS, heavy cycles, and bloating. Unlike GLP-1 drugs, which slow digestion dramatically, metabolic restoration speeds digestion in a way that supports sustainable fat loss and overall health.
The Real Solution Is Not Eating Less — It Is Metabolizing More
Weight loss becomes sustainable when the body can burn energy at a higher rate. This happens when thyroid function is strong, digestion is efficient, and dietary fat is not overwhelming the system. It happens when the metabolism feels safe, nourished, and warm. It happens when muscle is supported rather than wasted, when bile flows smoothly, when estrogen detoxifies properly, and when carbohydrates are being metabolized instead of feared.
GLP-1 drugs cannot create this environment. They can only suppress it.
Metabolic restoration, however, can transform it. When the body burns hotter and runs faster, weight loss becomes a natural, effortless extension of health rather than a fight against biology. This is why the answer is never long-term under-eating or slowing digestion. The answer is building a body that burns fuel easily, joyfully, and consistently — a body that has the metabolic flexibility and thyroid-driven energy it was always meant to have.
References:
GLP-1 RAs, delayed gastric emptying & long half-life (mechanism overview)
Shankar A, Chinthapalli S, Jose T, et al. Glucagon‐like peptide‐1 receptor agonists and delayed gastric emptying: implications for invasive cardiac interventions and surgery. Cardiovasc Endocrinol Metab. 2024;14(1):e00321.
https://pmc.ncbi.nlm.nih.gov/articles/PMC11620716/
GLP-1 agonists slow gastric emptying and small-bowel motility, have very long half-lives, and can leave food in the stomach despite fasting.
Clinical consequences of delayed gastric emptying on GLP-1s (human data)
Jalleh RJ, Plummer MP, Marathe CS, et al. Clinical Consequences of Delayed Gastric Emptying With GLP-1 Receptor Agonists and Tirzepatide. J Clin Endocrinol Metab. 2025;110(1):1–15.
https://academic.oup.com/jcem/article/110/1/1/7824836
Shows that delayed gastric emptying on GLP-1s is not just theoretical — they summarize evidence for retained gastric contents, aspiration risk, and altered nutrient handling with these drugs.
How much do GLP-1s actually slow gastric emptying? (meta-analysis)
Hiramoto B, McCarty TR, Lodhia NA, et al. Quantified metrics of gastric emptying delay by glucagon-like peptide-1 agonists: a systematic review and meta-analysis with insights for periprocedural management. Am J Gastroenterol. 2024;119(7):1126–1140.
This paper quantifies how much GLP-1s slow gastric emptying and discusses practical implications for procedures - this isn’t just appetite, it’s mechanical slowing of the gut.
Semaglutide: energy intake, appetite, and gastric emptying in obesity
Friedrichsen M, Breitschaft A, Tadayon S, et al. The effect of semaglutide 2.4 mg once weekly on energy intake, appetite, control of eating, and gastric emptying in adults with obesity. Diabetes Obes Metab. 2021;23(3):754–762.
https://pubmed.ncbi.nlm.nih.gov/33269530/
Use it for: direct evidence that semaglutide cuts calorie intake and slows gastric emptying rather than “fixing metabolism” — it’s appetite suppression + slowed gut transit, not a restoration of normal metabolic flexibility.
Weight regain after stopping semaglutide (STEP 1 extension)
Wilding JPH, Batterham RL, Calanna S, et al. Weight regain and cardiometabolic effects after withdrawal of semaglutide: The STEP 1 trial extension. Diabetes Obes Metab. 2022;24(8):1553–1564.
https://pubmed.ncbi.nlm.nih.gov/35441470/
After stopping semaglutide, participants regained most of the weight within a year and cardiometabolic markers drifted back toward baseline.
GLP-1s, endoscopy, and residual gastric contents (procedural risk)
Crespo J, Jiménez-García VA, Díez-Redondo P, et al. GLP-1 Receptor Agonists and Gastrointestinal Endoscopy. J Clin Med. 2025;14(15):5597.
https://www.mdpi.com/2077-0383/14/15/5597 MDPI
Discussion of higher rates of solid gastric residue and aspiration concerns in GLP-1 users during endoscopy. Slowed motility is clinically significant.
Low energy availability → low T3 + metabolic downshift (foundational thyroid piece)
Loucks AB, Callister R. Induction and prevention of low-T3 syndrome in exercising women. Am J Physiol. 1993;264(5 Pt 2):R924–R930.
https://pubmed.ncbi.nlm.nih.gov/8160876/
Shows that low energy availability itself (not just exercise) rapidly suppresses T3 and raises rT3, independent of thyroid gland disease. GLP-1-induced chronic undereating will push people toward a low-T3, low-metabolic state. Humans need a minimum of 43 cal/kg of LBM to be out of malnourishment. This is 2000-2500 cal for most women and close to 3000 for most men (with adequate muscle).
Microbiome, estrobolome & estrogen recirculation (for your estrogen detox angle)
Plottel CS, Blaser MJ. Microbiome and malignancy. Cell Host Microbe. 2011;10(4):324–335.
https://www.sciencedirect.com/science/article/pii/S1931312811002964
Introduces the “estrobolome” concept (gut microbes that deconjugate estrogens and recirculate them) and ties GLP-1-induced motility changes and reduced food volume to stagnant estrogen detox and higher estrogen burden.
The Metabolic Problem with Excess Protein
How Much You Really Need in Maintenance, Cutting, and Everyday Metabolism
Most people dramatically overestimate how much protein the human body can process without stress. High-protein diets have been promoted for decades in bodybuilding, fat loss programs, and low-carb circles, but the biochemical reality is far more nuanced. Excess protein—whether from muscle meat, eggs, dairy, whey, or even collagen—places a significant burden on the liver, raises stress hormones, increases serotonin, suppresses thyroid function, and shifts metabolism into a pattern that looks uncannily like low-grade hypothyroidism. Ray Peat spent years clarifying this misunderstanding: the body needs adequate protein, but excess is a metabolic liability, not an advantage.
This article walks through the science, numbers, and practical ranges for protein intake during bulking, cutting, and metabolic healing, all while integrating the Peat-aligned principles of oxidative metabolism, amino acid balance, CO₂ production, and thyroid physiology.
Why Excess Protein Is a Metabolic Stressor
When protein intake rises above the body’s anabolic needs, several predictable physiological mechanisms activate. The first is ammonia accumulation. Every amino acid that is not incorporated into tissue structure must undergo deamination in the liver. This produces ammonia, which is toxic, neurologically stimulating, and metabolically expensive to clear through the urea cycle. Ammonia load increases brain fog, irritability, fatigue, and mitochondrial inefficiency. The urea cycle is ATP-demanding, meaning excess protein indirectly lowers energy availability for tissues.
Protein also stimulates insulin without providing usable carbohydrate. When insulin rises in the absence of glucose, blood sugar falls. The result is a compensatory surge in cortisol and adrenaline, the two major catabolic stress hormones. This is why high-protein/low-carb diets produce anxiety, irritability, cold extremities, slow digestion, and insomnia. Cortisol blocks T4-to-T3 conversion in the liver, pushing thyroid physiology downward. Even when carbohydrates are present, very high protein loads still provoke higher basal cortisol as the body attempts to manage nitrogen waste and blood glucose stability.
Another problem is serotonin. All protein contains tryptophan, and Dr Ray Peat repeatedly emphasized that excess tryptophan and serotonin suppress mitochondrial respiration. Serotonin slows gastrointestinal motility, promotes inflammation, and interferes with thyroid hormone signaling. Even “clean” proteins like dairy, eggs, fish, and collagen contribute to tryptophan unless balanced by adequate carbohydrate and glycine. Excess protein of any form therefore increases serotonin load unless countered by a high-carbohydrate environment.
Protein oxidation also generates relatively low CO₂ compared to carbohydrate oxidation. CO₂ stabilizes cell metabolism, supports mitochondrial function, and maintains proper blood flow. Lower CO₂ from high protein intake means poorer oxidative metabolism, colder body temperatures, and a metabolic shift that resembles chronic stress. The high sulfur amino acids in protein (methionine, cysteine) raise homocysteine, antagonize thyroid function, and increase urinary calcium excretion.
Finally, high protein chronically activates mTOR, an anabolic switch that is useful in acute muscle-building contexts but harmful when persistently elevated. Chronic mTOR activation reduces autophagy and increases the risk for inflammatory and degenerative tissue states.
In short, excess protein increases ammonia, serotonin, nitric oxide, cortisol, liver burden, and thyroid suppression while decreasing carbon dioxide, oxidative metabolism, and metabolic stability. The modern obsession with ultra-high protein diets is not only unnecessary but counterproductive for metabolic function.
How Much Protein Is Actually Needed? The Peat-Aligned Range
Ray Peat consistently gave real-world numbers: most adults function best at 80–100 grams of protein per day, with 120 grams as the upper boundary for very large men. This is supported by nitrogen balance research showing that the human body saturates its protein synthesis capacity at relatively modest intakes. Above this threshold, the additional protein is burned for energy—or worse, converted into glucose through cortisol-dependent gluconeogenesis.
An 80–100 gram per day range provides enough amino acids for tissue repair, enzymatic function, detoxification, hormone transport, and structural maintenance. It avoids the ammonia burden and stress response that emerges at higher levels. It also supports thyroid function because the liver is not overwhelmed with excess nitrogen and sulfur processing.
Peat emphasized amino acid balance as much as total quantity. Approximately one-third to one-half of daily protein should come from gelatin, collagen, dairy proteins, or shellfish to balance the methionine-rich profile of muscle meat. Gelatin and glycine offset methionine’s inflammatory and thyroid-suppressive effects, lowering cortisol and supporting better sleep and digestion.
Protein Needs During Maintenance/Bulking: Not as High as You Think
Even during deliberate muscle-building phases, protein requirements do not rise dramatically. Research in resistance-trained adults demonstrates that maximal muscle protein synthesis occurs at approximately 1.6–1.8 g/kg of lean body mass—not total bodyweight. For a 70-kg individual with 55 kg of lean mass, this equates to roughly 90–100 grams of protein per day, aligning perfectly with Peat’s recommendations.
More protein does not mean more muscle. When carbohydrate intake is high and energy availability is adequate, muscles oxidize glucose efficiently and spare amino acids for repair and hypertrophy. The stimulus for muscle growth is resistance training plus energy surplus, not protein excess. As long as total calories are adequate and carbohydrates dominate fuel metabolism, 90–110 grams of daily protein is sufficient for hypertrophy.
Eating more protein than this does not accelerate growth. It increases ammonia, cortisol, and metabolic burden, ultimately slowing progress.
Protein Needs During Cutting: Lower Protein Preserves Metabolism
During energy restriction, the popular advice is to increase protein to “protect muscle.” The biology tells a different story. Very high protein during a cut increases cortisol because amino acids must be burned or converted to glucose in a calorie-deficient environment. Cortisol accelerates muscle breakdown and suppresses thyroid conversion, making fat loss harder and metabolic recovery slower.
Research from intermittent energy restriction models, MATADOR-style cycling, and athlete-based metabolic studies shows that maintaining normal—not elevated—protein intake preserves lean mass when carbohydrate intake is sufficient and energy availability is not chronically suppressed.
During a cut, Peat-aligned physiology works best around 0.9–1.2 g/kg of lean body mass. For many adults, this means 70–95 grams per day. Carbohydrates should remain high enough to maintain glycogen, support thyroid conversion, and blunt cortisol. Fat should remain low to preserve oxidative efficiency and prevent metabolic slowdown.
The key point is that protein does not need to rise during a cut. If anything, moderation protects thyroid function.
When to Eat More Protein (and When Not To)
Protein should rise modestly only when energy availability is high and carbohydrate intake is abundant. This occurs in:
deliberate bulking phases
high-calorie maintenance periods
periods of heavy resistance training with adequate sleep
Protein should not increase when:
calories are low
carbs are low
stress hormones are high
liver function is impaired
thyroid function is suppressed
digestion is compromised
These are the states where excess protein converts to cortisol, ammonia, serotonin, and stress.
The body thrives when carbohydrates are primary, protein is moderate and balanced, and fat remains the smallest energy contribution.
Conclusion
Excess protein is not harmless. It is metabolically expensive, thyroid-suppressive, and inflammatory when intake exceeds what the body can use for repair and enzymatic function. Ray Peat consistently emphasized that the optimal protein intake lies between 80 and 100 grams per day for most adults, with an upper boundary around 120 grams for large males. Even during muscle building, this range is sufficient when energy and carbohydrate intake are high. During cutting, protein should not increase; instead, it should remain moderate to prevent cortisol elevation and preserve thyroid function.
The modern fixation on very high protein diets contradicts both basic physiology and the energetically driven model of human metabolism. Moderation, balance, and carbohydrate dominance remain the most effective approach for metabolic resilience, thyroid support, and body recomposition.
References
Peat, R. various newsletters and interviews, Ray Peat Forum archives
Roddy, D. articles and interviews on metabolic and thyroid physiology
Haidut (Georgi Dinkov), Idealabs interviews and scientific commentary
Gorissen et al., "Protein requirements in trained individuals," Journal of Nutrition
Morton et al., "A systematic review on protein intake and resistance training," British Journal of Sports Medicine
Loucks, A. “Energy Availability and the Female Athlete,” Medicine & Science in Sports & Exercise
Bell et al., "Intermittent energy restriction and fat-free mass retention," International Journal of Obesity
We Weren’t Meant to Eat This Much Fat
Reclaiming Metabolic Health by Returning Fat to Its Proper Role
When most people picture ancestral diets, they imagine heavy meat consumption, rich animal fat dripping into fire, and a life of feasting on animal calories. But this image is misleading. For the majority of traditional societies studied by anthropologists, fat was not a staple fuel. It was rare, highly prized, and often consumed in the context of ceremonial feasts or seasonal abundance. Daily life was powered primarily by carbohydrates from fruit, tubers, honey, and other starchy plant foods, with lean animal protein supporting growth and repair. Fat was valued, but it was not the backbone of human nutrition.
The Carbohydrate Backbone of Ancestral Diets
One of the clearest examples of carbohydrate-based living comes from the Papua New Guinea Highlands. In this mountainous region, the sweet potato was not simply a side dish but the absolute centerpiece of the diet. Studies showed that the average adult consumed nearly one kilogram—about 956 grams—of sweet potato per day (Ohtsuka, 1983). That equates to more than 30 ounces, or three to five medium roots, yielding roughly 200 grams of carbohydrate.
But the sweet potato was not alone. Highlanders also consumed taro, yams, sugarcane, and bananas. Some surveys estimated that the total tuber intake exceeded 1000 grams daily, and that carbohydrate intake easily surpassed 500 grams per day. Energy intake in these populations has been estimated at 50–60 calories per kilogram of body weight, and yet obesity, diabetes, and cardiovascular disease were absent. These communities were lean, fertile, and active, with caloric intakes that would shock the modern dieter.
Protein came from small amounts of lean wild game, fish, or insects. Fat intake was extremely low, often under 10% of calories. Wild game typically contained only 4–7% body fat—far leaner than modern feedlot beef, which can exceed 30%. This alone reveals the distortion of our modern food supply: the fatty meat we take for granted was virtually absent in nature.
Feasts, Not Foundations
Fat did appear, but in a very different context. It was concentrated in ceremonial or celebratory feasts. In the Highlands, when a pig was slaughtered, the entire community gathered. For those few days, fat intake might soar to 30–40% of calories. Organ meats, marrow, and the precious fat were consumed in large amounts. But this was temporary. Once the feast ended, the population returned to their carbohydrate-rich baseline of sweet potatoes, taro, and bananas.
This rhythm shaped human biology. Fat was rare, so our brains evolved to crave it intensely when it appeared. Eating extra was adaptive—it provided survival insurance in uncertain food environments. But in the modern world, that ancient craving is constantly triggered. We live in a permanent feast, with processed foods delivering fat and sugar layered together at every corner store. This mismatch—ancestral scarcity versus modern abundance—explains why fat feels addictive and why moderation is so difficult.
The Eight Cultures Weston A. Price Studied
Nutrition pioneer Weston A. Price traveled the world in the early twentieth century, documenting the diets of traditional peoples. He identified eight cultures in depth. Seven thrived on diets that were low in fat and high in carbohydrates. The only exception was the Inuit, who lived in extreme environments with little plant food.
The Inuit diet, while high in animal fat, came with significant costs. Their fertility was lower, miscarriage rates higher, and life spans shorter than those of their high-carb counterparts. They experienced metabolic strain, and their survival strategy—relying on fat and protein in the absence of plant foods—was not an optimal diet, but a necessary adaptation to a harsh environment.
This is the critical lesson: high-fat, low-carb diets such as keto or carnivore are survival diets. They can sustain life when no other food is available, but they are not the ideal pattern for fertility, longevity, or metabolic resilience. Just as the Inuit accepted trade-offs to endure their climate, modern high-fat diets may help people endure short-term goals, but they come with long-term costs.
Humans Are Carbohydrate-Eaters
Biologically, humans are primates. And primates are overwhelmingly frugivores: fruit eaters. From chimpanzees to bonobos, primates thrive on fruit, tubers, leaves, and occasional small animals or insects. Humans are no different. Our physiology is built for carbohydrate metabolism.
The Hadza of Tanzania are a striking example. They consume honey ten months of the year, demonstrating that sweetness was a constant in the human story (Pontzer et al., 2018). Carbohydrates were never “junk” in an ancestral setting—they were the essential energy source that powered thyroid function, reproductive hormones, and brain activity. When we deprive ourselves of carbs, thyroid output drops, body temperature falls, and fertility declines. Carbohydrates are not optional; they are the fuel that drives human metabolism.
How We Got Lost: Tobacco Companies, Seed Oils, and Swampland
The modern diet is not the result of natural evolution but of corporate engineering. In the 1980s, tobacco companies such as Philip Morris (which bought Kraft and Nabisco) and RJR Nabisco (which absorbed General Foods) purchased food conglomerates. They applied the same playbook they had perfected with cigarettes: engineer products to maximize addiction.
The result was processed food that combined refined flour, sugar, and industrial seed oils. Americans were told to “fear carbs,” but most of the foods we casually label “carbs” are not carbohydrate foods at all. Pizza, donuts, cake, cookies, ice cream, nachos, and creamy pasta are 60-80% fat calories. These are hybrid foods: high fat plus moderate carbs.
This is swampland. Swampland is the zone where fat intake is high enough to block carbohydrate metabolism, while carbohydrate intake is still too low to protect thyroid and metabolic function. In swampland, fasting insulin rises, fat storage accelerates, and energy stalls. Seed oils exacerbate the problem, damaging mitochondria, thyroid hormone signaling, and cellular metabolism.
Everyone has their own “personal swampland,” the fat threshold at which their metabolism slows, insulin resistance appears, and weight creeps upward. Blood tests such as fasting insulin or HOMA-IR reveal when you’ve crossed into this territory. Carbs must be high enough to keep the system running. Fat must be low enough to prevent metabolic bog.
Fat as Dessert, Not Dinner
The ancestral lesson is clear: fat was never daily fuel. It was dessert, the rare feast food. Daily life was starch, fruit, honey, and lean protein. Fat was occasional, precious, and temporary.
To thrive today, we must relearn how to fall in love with carbs without fat. Real carbohydrate foods include fresh fruit and dried fruit, potatoes and other tubers, fruit juice, honey and maple syrup, lemonade and Italian sodas made with cane sugar, and—where tolerated—white rice, sourdough bread, sprouted oats, and masa harina tortillas. These foods deliver glucose without fat, fueling the thyroid and metabolism.
For modern application, keeping fat around 0.3 grams per kilogram of lean body mass—roughly 10–20 grams per day for women and 15–25 grams for men—functions as a reset phase, restoring insulin sensitivity and reversing weight gain. This can be sustained for one to two months, similar to the logic behind the Kempner Rice Diet. Long term, 0.5 g/kg makes a more sustainable baseline, with weekly or occasional feast days at 0.6–0.8 g/kg. This cycle mirrors the ancestral pattern: low fat most days, higher fat during rare feasts.
References
Ohtsuka, R. (1983). Nutritional adaptation of highland populations in Papua New Guinea. PubMed
Pontzer, H. et al. (2018). Energy expenditure and diet among Hadza hunter-gatherers. NCBI
Eaton, S. B., & Konner, M. (1985). Paleolithic nutrition. New England Journal of Medicine.
MDPI (2024). Worldwide hunter-gatherer diet macronutrient survey. MDPI
Chris Kresser. Kitavan macronutrient breakdown. Kresser
Pro-Metabolic Cancer Framework: Georgi Dinkov, Ray Peat, and the Real Story on Warburg
Metabolic Repair Before Oncologic Warfare
Ray Peat argued that cancer is fundamentally a disorder of impaired oxidative metabolism: when mitochondria can’t efficiently oxidize glucose, cells fall back on fermentation (lactate), stress chemistry rises, and growth signals run hot. His solutions emphasized restoring energy metabolism (adequate sugar/carbs, CO₂, thyroid support, anti-stress agents) rather than only attacking tumors head-on. Georgi Dinkov has popularized and extended this framework for a modern audience - continually pointing to low-risk, metabolism-supportive compounds (vitamins, aspirin/salicylates, caffeine, progesterone, etc.) that can shift metabolism back toward respiration while lowering pro-growth cytokines/prostaglandins. (For Dinkov’s own discussions, sample interviews here and here.)
The Warburg Effect—What It Is, and How It’s Misread
What Warburg observed: many tumors preferentially use glycolysis and make lactate even in the presence of oxygen (aerobic glycolysis). That observation—the Warburg effect—is not in dispute. Where it gets twisted: Warburg did not prove that “sugar feeds cancer.” He argued the mitochondria fail first, and fermentation follows. He thought defective respiration underlies the glycolytic shift; modern work shows a more nuanced reality—some cancers retain or even require mitochondrial respiration at different stages, and glycolysis/respiration usage varies with context and microenvironment. The takeaway: metabolism is reprogrammed, not simply “sugar in → cancer out.” Good reviews now emphasize both sides: the Warburg program provides growth advantages (biosynthetic flux, NAD⁺/NADPH management, immune evasion), yet restoring oxidative metabolism - or deprioritizing pathological glycolysis - can blunt malignancy. That’s the opening for pro-metabolic interventions.
B-Vitamins That Push Cells Toward Healthier Metabolism
Niacinamide (Vitamin B3)
Niacinamide (vitamin B3) helps refill NAD+, a core “battery” molecule your cells use to make energy. In lab and animal studies, this has slowed tumor cell growth and made abnormal cells more likely to self-destruct. It also tones down inflammation and supports safety-check genes like p53. Big picture: when NAD+ is adequate and the cell’s “electron balance” is steady, cells rely less on emergency fermentation (the sloppy sugar-burn that produces lactate) and more on clean, oxygen-based respiration—the direction you want if you’re trying to counter the Warburg pattern.
Thiamine (Vitamin B1)
Thiamine (vitamin B1) helps run PDH, the enzyme that acts like a gate - sending fuel (pyruvate) into the mitochondria to be burned cleanly with oxygen. When that gate works, less pyruvate gets turned into lactate, so lactate drops. In lab studies, high-dose thiamine slowed cancer-cell growth, cut their sugar use and lactate output, and made them more likely to self-destruct (apoptosis) - a pattern similar to the PDH-activating drug DCA. It’s preclinical (not proven in people), but it supports the “reverse Warburg” idea: push cells away from fermentation and back toward efficient respiration.
Aspirin & Simple Salicylates: Small Molecules, Big Metabolic Impact
Aspirin mostly works by turning down your body’s prostaglandin factory - the step cells use to make pain- and inflammation-messengers. It also calms sticky platelets and dials down a few stress switches inside cells, which can help mitochondria make cleaner energy. In people, long-term aspirin use is linked to lower risk of some cancers (strongest for colorectal), and that benefit seems to come from both the prostaglandin effect and other, deeper metabolic actions. Dinkov likes aspirin for exactly this profile: fewer inflammatory signals that push blood-vessel growth and tumor behavior, plus a nudge toward better respiration. Simple aspirin relatives - sodium salicylate and lysine acetylsalicylate - act similarly and have been used for years, though direct human proof of tumor shrinkage from these salts alone is limited. Bottom line: as part of a pro-metabolic plan, aspirin/salicylates can lower tumor-promoting prostaglandins and tilt cells toward healthier energy use - useful as an add-on to carb-adequate, thyroid-supportive nutrition. Just weigh the risks first (bleeding, ulcers, drug interactions).
The Broader Pro-Metabolic Toolkit (Peat/Dinkov Style)
Eating enough carbs with protein while keeping fats lower - especially seed oils - helps your thyroid run better, boosts carbon dioxide (a sign your metabolism is humming), and keeps you out of the stressed, adrenaline-driven “running on fumes” mode. Peat’s point is simple: more carbon dioxide and less lactate go hand-in-hand with healthier energy production. When it’s needed, thyroid/T3 helps cells use oxygen and burn sugar cleanly, instead of slipping into the backup “fermentation” mode that makes extra lactate. Basic light habits matter, too: bright morning light, steady sleep/wake times, and dark nights protect your energy-making machinery and lower stress hormones. And a few small helpers - caffeine (from coffee), glycine (from collagen/gelatin), vitamins D and K, and magnesium - tend to calm inflammation and support efficient energy use.
“Tumor Shrinkage” Claims With B-Vitamins + Aspirin—What’s Real?
The strongest evidence so far is from lab and animal studies. In those settings, niacinamide (B3) and thiamine (B1) can slow cancer-cell growth and sometimes push damaged cells to self-destruct. Aspirin has the best human signal and likely helps through more than one pathway, not just its well-known anti-inflammatory effect. Where the evidence is thin is in proving that vitamins alone shrink tumors in people; there are community stories, but solid clinical data are limited. Among these tools, aspirin/salicylates are the most supported in humans, but dose, timing, and personal risk (bleeding, GI issues, drug interactions) really matter. Bottom line: these approaches can tilt metabolism in a better direction and may work alongside standard care—but they are not stand-alone cures.
Practical Synthesis for a Pro-Metabolic Template
(Educational, not medical advice)
First, reframe Warburg: don’t fear carbs—fear broken respiration. Aim to restore oxidative metabolism and CO₂ while lowering lactate and inflammatory prostaglandins. Second, nudge metabolism upstream with adequate carbohydrate and protein, low PUFA, stable blood sugar, and abundant minerals; consider clinical evaluation of thyroid function if temps/pulse/symptoms suggest low metabolic rate. Third, use targeted adjuncts with the most evidence signals - niacinamide to normalize NAD⁺/redox and curb stress pathways, thiamine (B1) to favor PDH/mitochondrial entry and lower lactate, and aspirin/salicylates to suppress prostaglandins and support mitochondrial function - while balancing dose and risk. Finally, layer lifestyle levers such as bright morning light, consistent sleep, and gentle movement; each lowers stress metabolism and helps normalize immune function and respiration.
Final Word
Dinkov’s cancer-metabolism angle isn’t “magic vitamins.” It’s systems biology: reduce stress mediators, raise respiration and CO₂, keep blood sugar stable, and protect mitochondria. In that environment, tumors have fewer advantages. Preclinical evidence for B3, B1, and aspirin is real; human-level “tumor shrinkage” proof is incomplete but plausible as an adjuvant strategy - and it aligns with the plain-English metabolism markers we already track: pulse, temperature, sleep, mood, energy, digestion.
References
Liberti MV, Locasale JW. The Warburg Effect: How does it benefit cancer cells? Trends in Biochemical Sciences. 2016;41(3):211–218.
DeBerardinis RJ, Chandel NS. Fundamentals of cancer metabolism. Science Advances. 2016;2(5):e1600200.
Pavlova NN, Thompson CB. The emerging hallmarks of cancer metabolism. Cell Metabolism. 2016;23(1):27–47.
Rothwell PM, et al. Long-term effect of aspirin on colorectal cancer incidence and mortality. The Lancet. 2010;376(9754):1741–1750.
Thun MJ, Jacobs EJ, Patrono C. The role of aspirin in cancer prevention. Journal of the National Cancer Institute. 2012;104(20):1499–1506.
Chen AC, et al. A phase 3 randomized trial of nicotinamide for skin-cancer chemoprevention. New England Journal of Medicine. 2015;373:1618–1626.
Hanberry BS, et al. High-dose thiamine decreases proliferation and glycolysis in cancer cells. Integrative Cancer Therapies. 2014;13(5):409–417.
Bonnet S, et al. A mitochondria-K+ channel axis is suppressed in cancer; dichloroacetate normalizes metabolism and induces apoptosis. Cancer Cell. 2007;11(1):37–51.
Peat R. Cancer: Disorder and Energy. Essay/monograph; selected writings on respiration, lactate, and CO₂ in cancer.
Warburg O. On the origin of cancer cells. Science. 1956;123(3191):309–314.
Nebulizing Hydrogen Peroxide and Sea Salt: A Natural Remedy for Colds, COVID, and Lung Infections
Why Natural Healing Matters
Most respiratory illnesses—whether it’s a head cold, COVID, or a lingering lung infection—are viral in origin. Antibiotics don’t kill viruses, yet they are still widely prescribed, leading to unnecessary damage to the gut microbiome, fungal overgrowth, and antibiotic resistance. Instead of reaching for pharmaceuticals that often do more harm than good, there are safe, natural approaches that target the infection directly at its source. One of the most effective and accessible is nebulizing hydrogen peroxide and sea salt, with the option of adding a drop of iodine for extra antimicrobial support.
What is Nebulizing?
Nebulizing is the process of turning a liquid solution into a fine mist that can be inhaled deeply into the lungs and sinuses. This allows healing compounds to bypass the digestive tract and bloodstream and work directly in the respiratory system, where most pathogens first take hold. Because the therapy is localized, it can deliver powerful benefits without stressing the gut or overwhelming the rest of the body.
The Healing Formula
This simple yet powerful solution can be mixed right at home. In a clean glass jar, combine:
8 ounces (1 cup) of distilled, sterile, or purified water
2 teaspoons of 3% food-grade hydrogen peroxide
½ teaspoon finely ground sea salt
Stir until fully dissolved. Store the solution in the refrigerator for up to one week.
To use, pour 1–2 teaspoons of the mixture into your nebulizer cup. Optional: 1 drop of Lugol’s 2% iodine can be added to the nebulizer cup itself.
Place the mask or mouthpiece over your nose and mouth and inhale the mist slowly and deeply for 5–15 minutes. This can be done once to three times daily at the onset of illness, then tapered as symptoms improve.
Why This Formula Works
Hydrogen peroxide is not a foreign chemical—it is a molecule the body itself produces as part of the immune response. White blood cells generate hydrogen peroxide to kill pathogens. When used in safe, dilute concentrations, inhaled peroxide mimics this natural defense, breaking down viral envelopes, dismantling bacterial biofilms, and oxygenating tissues that are inflamed or struggling to heal. This direct delivery system gives the immune system an advantage right where the infection is happening.
The sea salt in the mixture does more than soothe the airways. Salt is also a potent antimicrobial agent. It creates a hypertonic environment that pulls water out of bacteria and fungi through osmosis, dehydrating and killing them. This is the same principle behind traditional salt preservation of foods. In the respiratory tract, added salinity helps reduce microbial load, discourage overgrowth, and support tissue repair. Salt also thins mucus, hydrates the airway lining, and makes it easier for the body to expel congestion.
For those who choose to add iodine, the benefits expand even further. Iodine has long been used as a broad-spectrum antiseptic, capable of neutralizing viruses, bacteria, and fungi within seconds in lab settings. Adding just one drop to the nebulizing solution provides an extra layer of defense without overwhelming the system.
Together, hydrogen peroxide, sea salt, and iodine form a multi-pronged natural therapy. They oxygenate and disinfect the respiratory tract, kill pathogens directly, break down mucus and biofilms, and support the body’s own innate defenses. Unlike antibiotics, which are narrow in scope and destructive to the microbiome, this approach works with the body to restore balance and healing.
When and How to Use It
The nebulizing solution can be used at the first sign of a head cold, sore throat, or congestion. Many people find it especially effective for reducing viral load in cases of COVID and other respiratory viruses, easing symptoms and shortening duration. It is also beneficial for stubborn bronchitis, lingering coughs, or chronic sinus congestion, where biofilms and mucus buildup are often part of the problem.
During acute illness, one to three sessions per day can help bring relief quickly. Once symptoms begin to resolve, the therapy can be tapered down to once daily or discontinued altogether. Because this is a localized and supportive therapy, it can be repeated as needed whenever viral or bacterial respiratory issues arise.
Safety Considerations
Always use food-grade hydrogen peroxide, never the brown-bottle drugstore version, which contains stabilizers and impurities that are unsafe to inhale. Stick to the formula’s exact dilution—more is not better, and stronger concentrations can cause irritation. If you notice burning, coughing, or sensitivity, reduce the session length or frequency. While this therapy is safe for most adults, it is not recommended for infants or very young children unless under the supervision of a practitioner.
Final Word
Respiratory infections are a fact of life, but antibiotics don’t have to be the default. By using a safe and time-tested protocol like nebulizing hydrogen peroxide, sea salt, and optional iodine, you can directly address pathogens in the airways, support the body’s natural healing mechanisms, and restore balance without disrupting the gut or relying on pharmaceuticals. This simple formula may look humble, but its ability to oxygenate, disinfect, and heal makes it one of the most powerful remedies to keep on hand for colds, COVID, and lung infections.
References
Jockers, D. (2020). Nebulizing Peroxide: A Powerful Healing Therapy. DrJockers.com. https://drjockers.com/nebulizing/
Brownstein, D. (2020). Clinical experience with nebulized hydrogen peroxide for respiratory infections. Case reports.
Caruso, A. et al. (2020). Povidone-iodine nasal/oral antiseptics effective against SARS-CoV-2 in vitro. Infect Dis Ther, 9(4), 915–924.
Bidra, A. S. et al. (2020). Rapid in-vitro inactivation of SARS-CoV-2 using povidone-iodine rinse. J Prosthodont, 29(6), 529–533.
Reimer, L. et al. (2008). Antimicrobial properties of hypertonic saline. J Appl Microbiol, 105(6), 1805–1813.
Escaping Swampland: Why Healing the Body Means Returning to High Carbs
Across Evolution, Carbs Have Always Been The Foundation Of Human Energy
Modern humans are drowning in what Denise Minger calls Swampland nutrition — the deadly combination of refined fats and refined carbohydrates eaten together. Think of chips, donuts, fries, pastries, pizza, and ice cream. These foods didn’t exist in nature. For seven million years of primate and human evolution, we either ran on carbs or on fat — but never equal amounts of both at once, and never with over half the fat coming from seed oils. This distinction matters for metabolism, thyroid health, and body composition today.
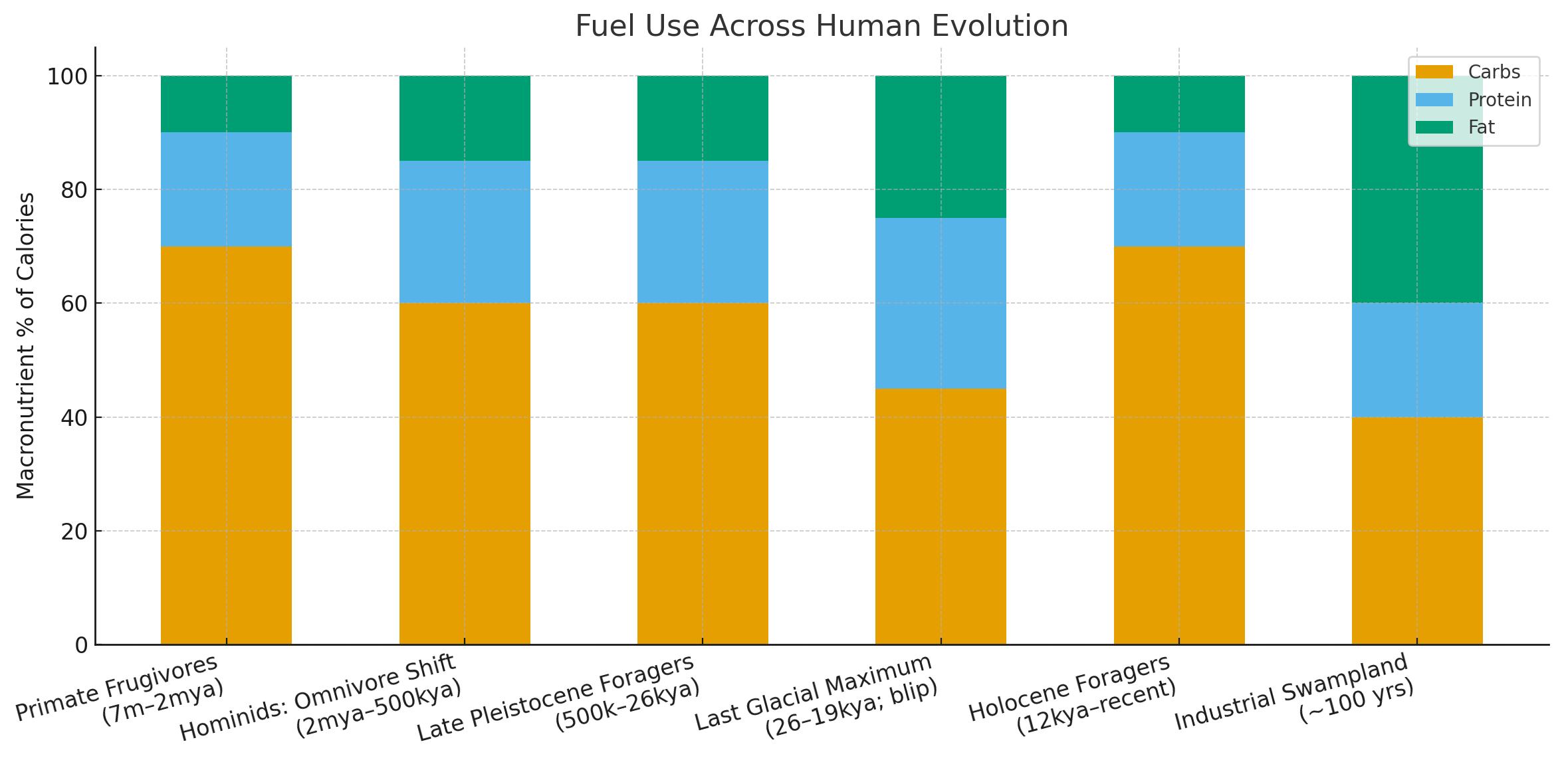
The Evolutionary Fuel Story
Our story begins with our primate ancestors. For roughly 7 million years, chimpanzees, bonobos, and early hominins were overwhelmingly fruit eaters. Their diets centered on fruits, tubers, and other carbohydrate-rich plants, with protein from leaves and insects and modest amounts of fat from fruit seeds and the natural byproducts of fermenting fiber. For more than 90% of our evolutionary history, humans and our relatives were fundamentally carb-burners.
Around 2 million years ago, the first biped hominids (members of the genus Homo) began to emerge from the trees and walk on two legs. This is when a true dietary shift occurred: from being mostly frugivores to becoming omnivores. These early hominids began actively consuming animals — not just insects, but scavenged and hunted mammals. This added more protein and some fat to their diets, though it’s important to note that fat was still limited. Most wild animals are relatively lean, with body fat percentages ranging from about 4–7% in small to medium animals, and only slightly higher in certain larger species.
During the Ice Ages, especially in northern latitudes, humans occasionally encountered (and learned to hunt) megafauna such as mammoths, mastodons, and giant bison. This was largely during the last Glacial Maximum, starting 26,000 years ago. These animals carried somewhat higher fat reserves, especially seasonally, and they provided a crucial energy source in environments where plant foods were scarce. But this period of heavier reliance on animal fat was a short blip in evolutionary time, not the norm. Even then, the majority of humans lived closer to the equator, where tubers, fruits, and honey remained reliable staples.
By about 12,000 years ago, most of the megafauna had gone extinct. Fat-rich prey largely disappeared, and humans turned back toward plants for the bulk of their energy. Foragers and early farmers relied heavily on tubers, palm starch, fruits, honey, and eventually grains. Fat and protein intake fell, and carbohydrates once again became the foundation of the human diet. Agriculture locked this in further. For most of recorded history, humans were primarily carb-burners.
Only in the last 100 years did something truly novel appear: industrial Swampland foods. For the first time, humans combined high fat and high carb simultaneously. Refined flour and sugar mixed with industrial seed oils created the metabolic swamp we live in today. Modern diets now feature unusually high fat intake — much of it unstable polyunsaturated oils — alongside refined, nutrient-poor carbs. Protein has shrunk, and metabolism has slowed.
Why Swampland Breaks the Human Metabolism
Our mitochondria handle one main fuel stream at a time. When both carb and fat are high, insulin pushes carbs into cells, but fat oxidation stalls. Excess fatty acids — especially linoleic acid and other unstable PUFAs — flood the bloodstream and compete directly with glucose at the mitochondrial level, a phenomenon known as the Randle Cycle. This competition blocks glucose oxidation, leaving sugar trapped in the blood while cells are forced to rely on fat. The mismatch creates insulin resistance and keeps blood sugar elevated. Eventually, the pancreas overshoots with extra insulin, driving blood sugar down too far and triggering reactive hypoglycemia — the shakiness, anxiety, and fatigue so many people feel after eating Swampland foods. Over time, this chronic tug-of-war between fat and carbs damages mitochondria, suppresses thyroid hormone action, and locks in long-term insulin resistance. The result is a cascade toward obesity, low body temperature, infertility, depression, and chronic fatigue.
In contrast, carb-dominant diets — low fat, high carb, adequate protein — keep the thyroid humming, temperatures warm, and metabolism high. When fat is kept low, glucose flows freely into the cell without competition from fatty acids. This lowers the burden on insulin, restores metabolic flexibility, and reverses the mitochondrial gridlock of the Randle Cycle. Instead of swinging between high blood sugar and reactive hypoglycemia, the body maintains a steady supply of fuel to the brain and muscles. The thyroid responds by converting more T4 into active T3, raising body temperature and stabilizing mood, sleep, and energy. Over time, this translates into more resilient hormone balance, easier fat loss, and a metabolism that runs at a higher “idle speed.”
By contrast, fat-dominant diets can work short-term — especially during food scarcity, when survival depends on stored body fat. But when pursued long-term, the cost becomes clear: thyroid conversion slows, reproductive hormones drop, body temperature cools, and energy output declines. The body is forced into conservation mode, trading short-term survival for long-term vitality. This is why so many people on extended keto or carnivore notice hair loss, menstrual irregularities, PMS and menopause symptoms, muscle aches, constipation, low libido, fatigue, headaches, insomnia, or slowed fat loss despite strict discipline. It’s not a failure of willpower — it’s the physiology of a body running on the wrong primary fuel.
Why High-Carb, Low-Fat Is the Healing Path Now
For people coming out of years of keto or carnivore, the damage is often visible. They experience suppressed thyroid function with cold hands and feet, low body temperatures, and fatigue. Insulin resistance persists, fueled by stress hormones and PUFA-rich fat stores. Many struggle with body composition despite their discipline.
The way out isn’t to double down on fat. It’s to return to our evolutionary baseline: carbs as the primary fuel, with fat kept low enough to force the body to oxidize carbohydrate efficiently.
Shifting back to carbs has multiple benefits. Carbs stimulate T3 production and rebuild metabolic rate. Very low-fat, high-carb eating reverses insulin resistance faster than any other approach. Glucose availability supports reproductive hormone balance, while higher carb intake with adequate protein preserves muscle and promotes fat loss. In short, it rebuilds metabolism at the cellular level.
Practical Application
The healing path is simple. Keep carbohydrates high, sourced from fruit, honey, juice, sugar, tubers, and properly prepared grains. Keep fat low while strictly avoiding PUFA from seed oils. Maintain protein at adequate levels by prioritizing lowfat dairy, lean meat, gelatin, and collagen. Over time, this allows the body to burn off old PUFA stores and restore efficient carb metabolism.
The Big Picture
For seven million years, humans and our primate cousins thrived as carb-burners, with only a brief Ice Age detour into fat-burning thanks to megafauna. What we never adapted to is the modern swamp: high fat and high carb together. If you’re recovering from keto or carnivore, struggling with insulin resistance, thyroid issues, or stubborn weight, the solution is not to double down on fat-burning. It’s to reclaim your natural carb-fueled metabolism and escape the swampland for good.
Healing the metabolism starts by simplifying fuel. Stop drowning in Swampland. Return to carbs, lower fat, and watch your body remember how to thrive again.
References
Lee-Thorp, J. & Sponheimer, M. (2006). Contributions of stable isotopes to understanding diet and ecological adaptation of early hominins. Journal of Human Evolution.
Richards, M. & Trinkaus, E. (2009). Isotopic evidence for the diets of European Neanderthals and early modern humans. PNAS.
Wood, B. & Hawkes, K. (2017). Human evolution: Dietary ecology. Annual Review of Anthropology.
Krigbaum, J. (2003). Reconstructing human subsistence with stable isotopes in tropical contexts. Asian Perspectives.
Roberts, P. & Petraglia, M. (2015). Palaeolithic adaptations in tropical forests. Journal of Human Evolution.
Hill, K. & Hurtado, A. (1996). Aché Life History: The Ecology and Demography of a Foraging People. Aldine de Gruyter.
Thyroid Health, Weight Loss, and the Power of Carbs
Introduction: Why Thyroid Health Matters
Most people think of thyroid dysfunction as a niche medical issue. In reality, your thyroid is the master regulator of energy. When it slows, every system in your body slows with it — digestion, mood, fertility, fat loss, and even your ability to feel warm.
Unfortunately, modern medicine often overlooks the full scope of hypothyroidism because it relies too heavily on blood tests like TSH. These markers miss what’s happening at the cellular level, where T3 — the active thyroid hormone — determines whether your cells make ATP (energy) or limp along half-starved.
How the Thyroid Works: TSH → T4 → T3 → rT3
The thyroid system runs on a conversion pathway:
TSH (Thyroid Stimulating Hormone): Produced by the pituitary, it tells the thyroid gland to release hormones. Think of TSH as mailing a letter.
T4 (Thyroxine): The storage form, released in larger amounts but biologically inactive. This is the letter arriving in the mailbox.
T3 (Triiodothyronine): The active form, converted from T4, drives cellular energy production. This is the letter getting opened and read.
rT3 (Reverse T3): A “dead-end” hormone made from T4 under stress, starvation, inflammation, or toxin load. This is the letter being returned to sender, clogging up the mail system.
When you’re under stress, cutting calories, or eating low-carb, conversion skews toward rT3. Labs may look “normal” (TSH and T4 in range) while you remain cold, tired, and unable to lose weight — the classic picture of functional hypothyroidism.
The Three Types of Hypothyroidism
Functional Hypothyroidism – driven by stress, low calories, low carbs, toxins, or high rT3. Reversible with lifestyle, nutrition, and sometimes T3 support.
Autoimmune Hypothyroidism (Hashimoto’s) – caused by immune attack on the thyroid gland. Often linked to viral triggers, gut dysfunction, mold, and environmental toxins.
Nutrient-Deficiency Hypothyroidism – caused by lack of cofactors like iodine, selenium, iron, copper, or B vitamins that are necessary for thyroid hormone synthesis and conversion.
Understanding which type (or combination) you’re dealing with is critical for treatment.
Food First: Carbs, Calories, and Detoxification
The thyroid can’t function without fuel. Restricting calories or carbs is one of the fastest ways to suppress T3. Research shows that carbohydrate deprivation directly inhibits the conversion of T4 to T3, leaving you with “normal” bloodwork but classic hypothyroid symptoms — fatigue, hair loss, depression, constipation, cold hands and feet.
Long-term, the best path to thyroid restoration is:
Adequate calories (at least 43–48 kcal/kg lean body mass for recovery).
High carbohydrates (fruit, juice, honey, tubers) to maintain glycogen and conversion to T3.
Low PUFA (polyunsaturated fats) to reduce thyroid-blocking effects at the cellular level.
Detox pathways – supporting the liver to clear excess estrogen, endotoxin, and heavy metals that impair thyroid conversion.
Body Temperature and Pulse as Markers
Body temperature and pulse are simple at-home measures of thyroid status. Ideally:
Waking temp: ~97.8°F
Post-breakfast temp: ~98.6°F
Resting pulse: 75–85 BPM
If temps drop after eating, stress hormones (like cortisol and adrenaline) are running the show, not thyroid.
NDT vs. T3: Why Medication Matters
Historically, Natural Desiccated Thyroid (NDT) was the treatment of choice. It contains both T4 (the pro-hormone) and T3 (the active hormone). For many, NDT restores warmth, energy, and weight regulation.
But in others, the T4 portion fails to properly convert to T3, especially under stress, low-carb dieting, or liver burden. That’s when people experience the classic “NDT stopped working for me” story.
In those cases, small, frequent doses of T3-only (like Cynomel) can be more effective. T3 bypasses the conversion bottleneck and directly fuels the cell. The key is microdosing with meals, not blasting the system with one big dose.
Some people do best with a combination of NDT and added T3, ensuring both storage hormone (T4) and active hormone (T3) are available. Others thrive on T3-only protocols, especially when conversion is chronically impaired. The right approach depends on labs, body temperature, pulse, and symptoms — not TSH alone.
Fat Intake and Our Ancestors
Another overlooked piece is fat intake. Modern Western diets often hover at 35–40% fat, with much of it from unstable seed oils. Historically, many traditional diets hovered closer to 10–15% fat. Excess dietary fat — especially polyunsaturated fats — interferes with thyroid hormone transport into cells and slows metabolism.
The Inuit are often cited as thriving on high-fat diets, but history tells a different story. For much of the year, their fertility rates were very low. Births only increased during the short season when they consumed fresh animal thyroid glands, boosting thyroid function. Without carbs or thyroid tissue, their metabolism and reproduction suffered.
In other words: fat alone didn’t sustain them. Thyroid did.
Weight Loss Through a Thyroid Lens
For those struggling with weight loss, thyroid optimization is not optional. You can slash calories and lose weight, but if thyroid function is low, you’ll mostly burn through muscle and stress hormones, not fat. True fat loss comes when metabolism is high enough that your body feels safe to burn stored energy.
That means:
Enough carbs to keep glycogen full.
Adequate calories (at least 43–48 kcal/kg lean body mass for recovery).
Low PUFA, moderate protein, and modest fat (10–20%) to reduce metabolic drag.
Thyroid support (NDT, T3, or both) if labs, temps, and symptoms show you’re running cold.
Closing Thoughts
Hypothyroidism isn’t just about a sluggish thyroid gland. It’s a systemic problem of low energy production. Starving yourself of carbs, overloading fat, or leaning too hard on T4-only medication all drive the same outcome: cold, tired, infertile, overweight, and stuck.
NDT and T3 supplementation can be powerful tools, but they are best seen as temporary supports. These medications are not foreign chemicals — they are identical to the hormones your body is supposed to make. When stress, poor diet, toxins, or years of under-eating have reduced your own production and conversion, supplementing provides what’s missing so your cells can actually make energy. While you rebuild metabolism with adequate calories, high carbs, low PUFA, and detoxification, thyroid meds help keep your body warm and energized enough to burn fat instead of leaning on stress hormones. Once metabolism is restored, many people can taper off medication and rely on food, lifestyle, and nutrient sufficiency for long-term thyroid health.
References
https://academic.oup.com/edrv/advance-article/doi/10.1210/endrev/bnaf015
https://www.nature.com/articles/s41598-019-41997-2
https://restorativemedicine.org/journal/peripheral-thyroid-hormone-conversion-and-its-impact-on-tsh-and-metabolic-activity/
https://pubmed.ncbi.nlm.nih.gov/1249190/
https://pubmed.ncbi.nlm.nih.gov/11167929/
https://pmc.ncbi.nlm.nih.gov/articles/PMC11314468/
https://pmc.ncbi.nlm.nih.gov/articles/PMC5793233/
https://pubmed.ncbi.nlm.nih.gov/30020/
https://pmc.ncbi.nlm.nih.gov/articles/PMC4044302/
https://pubmed.ncbi.nlm.nih.gov/11167929/
https://pmc.ncbi.nlm.nih.gov/articles/PMC4044302/
https://www.thyroid.org/patient-thyroid-information/ct-for-patients/vol-6-issue-8/vol-6-issue-8-p-3/
https://bmcendocrdisord.biomedcentral.com/articles/10.1186/s12902-024-01612-6
How to Eat Out at Restaurants
…Without Wrecking Your Metabolism or Your Gut
Eating out doesn’t have to derail your health goals—if you know what to look for. Restaurants are notorious for relying on cheap seed oils, mystery sauces, and low-quality meats, but with the right mindset and a few simple strategies, you can walk away nourished instead of inflamed.
Mindset First: Control What You Can
Perfection isn’t realistic at a restaurant, but upgrades are. The goal isn’t to replicate a home-cooked pro-metabolic meal—it’s to avoid the biggest offenders while making the best of what’s available. Focus on real food over processed fillers, keep seed oils out whenever possible, choose digestion-friendly meals, and balance your blood sugar with protein, carbs, and real dairy.
Best Restaurant Types for Pro-Metabolic Eating
Breakfast diners are often the easiest place to eat clean. You can order three eggs cooked in butter (or dry and add your own), fruit, potatoes, sourdough toast with jam or honey, and fresh orange juice or milk. Steakhouses are another safe bet, offering lean cuts of beef or steak, baked potatoes, and seasonal veggies that can usually be cooked in butter instead of oils.
Authentic Mexican restaurants can work well if you stick to corn masa tortillas, grilled beef, rice, cheese, and crema while avoiding fried chips and vegetable-oil-heavy sauces. Greek and Mediterranean spots are great for lamb, beef, rice, goat cheese, tzatziki, and olives, though you’ll need to confirm whether they’re using olive oil or canola. Sushi and Japanese restaurants are excellent for rice, cooked fish, tamago (egg), seaweed, and fresh fruit. Poke bowls are especially flexible—you can build one with plain rice, shrimp or tuna, avocado, and fruit while skipping the tempura and mayo-based sauces.
Vietnamese restaurants are another underrated option. Vermicelli noodle bowls with shrimp or beef, fresh herbs, and veggies can be a clean, filling choice if you ask for your protein cooked without oil and skip the seed-oil dressings. Pho can work too if the broth is clean and you choose beef or shrimp over pork. Finally, farm-to-table restaurants are often open to special requests and may even celebrate them. Many will cook in butter or olive oil if asked, and desserts based on fruit instead of flour are common.
What to Watch Out For
The biggest red flag in nearly every restaurant is seed oils. Anything fried, sautéed, or dressed in salad dressing is almost guaranteed to be drenched in canola, soy, or soybean oil. Low-quality pork and chicken are another issue since they’re high in PUFAs and rarely worth it. Sauces are another metabolic landmine, often containing soy, cornstarch, MSG, gums, and oils. Breadings, gravies, and pasta sauces usually add fillers without any nutritional benefit.
Best Menu Choices
At breakfast or brunch, stick to eggs cooked in butter or dry, fruit, plain or buttered potatoes, and sourdough toast with honey or jam. Yogurt parfaits can work if you check for added sweeteners and avoid commercial granola. Fresh-squeezed juice or milk , as well as coffee with skim milk and honey make for great beverage options.
At lunch, a burger patty with real cheddar cheese and a side of fruit or baked potato is a clean choice. Salads can be modified—such as a Caesar without dressing, topped with olive oil and lemon instead, and made with real parmesan. Sandwiches on sourdough work, or gluten-free white bread in a pinch.
Dinner options are usually straightforward: grilled steak or fish with a baked potato and seasonal vegetables, a rice bowl with meat and fruit sides, or tacos on corn tortillas with beef, crema, and salsa. American restaurants make this easy—you can always ask for a plain burger patty with real cheese, a steak with baked potato, or a cup of fruit for dessert. Even chain places like Dairy Queen have decent options—a pineapple smoothie is metabolically friendlier than a diet soda, and a scoop of real ice cream beats sugar-free desserts filled with gums and chemicals. Sushi, poke bowls, and even simple diner plates can all be adjusted into pro-metabolic meals.
Practical Tactics
The best thing you can do is ask directly how the food is cooked. A simple, “Can you cook this in butter instead of oil?” usually works. If you don’t see anything that fits your needs, order off-menu with a request like, “Plain grilled steak, a baked potato, and fruit.” Keeping a small jar of honey, a travel sea salt shaker or even butter packets in your bag makes it easy to upgrade meals.
Most importantly, don’t be afraid of sugar. Choosing fruit, juice, or even a scoop of ice cream is metabolically safer than seed-oil fried desserts or sugar-free chemical options.
Pro-Metabolic Extras
Not every restaurant is a seed-oil minefield—some actually surprise you with great options. A few pizzerias now make sourdough or gluten-free rice flour crusts, which are far easier to digest than the usual wheat-based versions loaded with additives. Some higher-quality restaurants are also switching their fryers from vegetable oil to beef tallow or other traditional fats—if you find a place that does, it’s a major win.
Desserts can often be hacked too. Instead of going for heavy cakes or fried sweets, ask for pie and don’t eat the crust or a simple scoop of real ice cream with fruit. These small tweaks keep things pro-metabolic without feeling deprived.
And sometimes, the best restaurant alternative is skipping the restaurant altogether. If you’re traveling or just don’t feel like compromising, stop at a grocery store, grab a few clean staples like fruit, sourdough, cheese, and deli meat, and make your own dinner in a park. It’s cheaper, often tastes better, and guarantees you’re eating within your own standards.
Summary
When eating out, don’t aim for perfection—just avoid the metabolic landmines. Seed oils, fried foods, and mystery sauces are the biggest problems. Choose butter, olive oil, or dry cooking. Stick with lean meats, fruit, potatoes, sourdough, and real dairy, and don’t hesitate to ask for what you need.
Eating out can actually be enjoyable and safe for your metabolism when you know how to order.
Specific Eating-Out Guide:
Real-World Guide: What to Order at Restaurants (Pro-Metabolic Edition)
Eating out doesn’t have to mean wrecking your metabolism. The trick is to avoid seed oils, fried foods, and mystery sauces while building meals around protein, fruit, starch, and real dairy. Here’s a breakdown of exactly what to order at different restaurants so you can eat out confidently and still feel good afterward.
Chipotle
Chipotle is a solid choice, but every meat is cooked in some oil, so it’s not perfect. The best option is barbacoa since it is boiled and tends to be less oily than chicken or carnitas. Pair it with white rice, a small sprinkle of cheese, a spoon of sour cream, salsa, and maybe a little guacamole if you want extra calories. Skip the fajita veggies (cooked in seed oils) and avoid the tortillas and chips since they’re cooked in soybean oil. A bowl is always safer than a burrito.
Diners & Breakfast Spots
Classic diners are some of the easiest places to upgrade. Ask for three eggs cooked in butter or dry, a baked or hashbrown-style potato (no oil), fruit on the side, and sourdough toast with honey or jam. If they don’t have sourdough, just skip the bread instead of eating commercial white bread. Milk or fresh orange juice are great, as well as coffee with milk and sugar.
Sushi & Japanese
Sushi is one of the cleanest cuisines if you avoid fried tempura and mayo-based rolls. Go for simple rolls with white rice, cooked fish, shrimp, tamago (egg), or tuna/salmon. Poke bowls are fantastic—choose plain white rice, shrimp or tuna, avocado, seaweed, fruit, and light soy-free toppings. Avoid fried sides, fake crab (often mixed with canola mayo), and “spicy mayo” sauces. Even a miso soup and plain rice combo with sashimi works as a safe meal.
Steakhouses
This is where eating pro-metabolic feels luxurious. Order a grilled steak or shrimp cooked in butter (or ask for dry cooking and add butter yourself), a baked potato with sour cream, fruit or a veggie side, and maybe a small scoop of ice cream if they offer it. Steakhouses usually have higher-quality cuts of beef, and baked potatoes with butter are a metabolic win.
Mexican (Authentic, Not Chains)
Look for tacos on corn tortillas with grilled beef, cheese, crema, and salsa. Rice and beans are fine if beans don’t bother your digestion. Skip fried tortilla chips (seed oil central) and oily salsas. At higher-quality spots, a plate of carne asada with rice and avocado is a clean order.
Vietnamese
Vermicelli noodle bowls are great—ask for shrimp or beef not grilled in oil, fresh herbs, veggies, and sauce on the side (since many dressings are made with vegetable oils). Pho can also work if the broth is clean and you choose beef or shrimp instead of fatty pork.
Mediterranean
A safe bet here is grilled lamb or beef with rice, tzatziki, goat cheese, and olives. Just confirm if they’re using olive oil or canola. Skip the deep-fried falafel and oily dolmas. A Greek salad with feta, olives, cucumber, and lemon juice works well if you leave off the dressing.
Farm-to-Table
These restaurants are usually the most accommodating. Order seasonal meat or fish cooked in butter, a baked potato or root veggie, and fruit or a fruit-based dessert. Most chefs at these places appreciate a clean, simple request.
American Chains
Even American chain restaurants can work if you know what to ask for. At a sit-down chain, order a plain burger patty with cheddar cheese (no bun, no fries) and swap sides for a baked potato, cup of fruit, or a salad with olive oil and lemon. Steak with baked potato is another easy order. If dessert’s on the table, a scoop of real vanilla ice cream or pie filling is far better than sugar-free chemical options.
Fast Food (In a Pinch)
Fast food isn’t ideal, but there are upgrades. At Dairy Queen, a pineapple smoothie is surprisingly cleaner than many drinks, and a small vanilla cone beats any sugar-free “dessert.” At McDonald’s or similar places, the best option is usually burger patties with cheese, pickles, and mustard (no bun, no sauces, no fries) plus milk, espresso, or juice. It’s not perfect, but it’s lower PUFA than fried items.
Final Thoughts
Eating out doesn’t have to sabotage your metabolism. Every menu has something you can work with if you focus on butter over oil, plain proteins, baked potatoes or rice, fruit, and real dairy. Don’t stress about perfection—upgrading your choices makes a huge difference. And remember: a scoop of real ice cream is always better than seed oil fried desserts or “sugar-free” chemical alternatives.
The Estrogen Burden: How to Rebuild Your Hormones from the Root
Fixing Estrogen Dominance with Food, Light, and Bioidentical Support
If you’re tired, puffy, anxious, bloated, emotionally volatile—or stuck in a body that no longer feels like yours—your hormones may be trying to get your attention. Estrogen dominance is one of the most common, least understood drivers of metabolic dysfunction today. It affects both women and men, and it’s not just about how much estrogen you have—it’s about the lack of opposing forces like progesterone, pregnenolone, and thyroid hormone.
We live in a world that constantly pushes our bodies into stress mode. Under those conditions, estrogen takes over—and everything else falls apart.
What Is Estrogen Dominance?
Estrogen dominance means estrogen is elevated relative to other key hormones—especially progesterone in women and testosterone in men. It can show up even when bloodwork looks “normal,” because the problem isn’t always how much estrogen you have. It’s how well you detox it, how inflamed your tissues are, and how much protective opposition you have from other steroid hormones.
Symptoms of estrogen dominance include:
Weight gain and fluid retention
PMS, breast tenderness, endometriosis, or heavy cycles
Mood swings, anxiety, insomnia, and brain fog
Low libido and infertility
Fatigue, low muscle tone, and slowed metabolism
“Dad bod,” gynecomastia, or erectile dysfunction in men
This state isn’t just uncomfortable—it’s metabolically suppressive. Estrogen slows thyroid function, raises cortisol, impairs bile flow, and makes the body less efficient at burning fat or building lean tissue. It keeps you stuck in a stress response—while pretending to be your reproductive ally.
Why Modern Life Pushes Us Into Estrogen Dominance
Estrogen dominance used to be rare. But today, most people are swimming in it—thanks to a perfect storm of stress, toxins, poor light exposure, and broken metabolism.
Key contributors include:
PUFAs (polyunsaturated fats): These oils block thyroid hormone, increase estrogen signaling, and suppress mitochondrial energy production.
Xenoestrogens: Found in plastics, fragrances, receipts, pesticides, and birth control—they mimic estrogen and overwhelm your detox pathways.
Low-carb or low-calorie dieting: Chronic under-eating downregulates progesterone, pregnenolone, and thyroid hormone.
Liver and gut dysfunction: Impaired bile flow or gut dysbiosis leads to poor estrogen clearance and recirculation.
Chronic stress: Your body diverts pregnenolone into cortisol (the “pregnenolone steal”), starving your sex hormones and locking you in survival mode.
This hormonal pattern shows up in bloodwork as normal or even low estrogen—but the body is drowning in estrogenic activity at the tissue level. That’s why so many people are estrogen dominant without realizing it—and why they don’t get answers from conventional hormone panels.
Progesterone: The Hormone That Brings You Back to Life
Progesterone is more than just a “female hormone.” It’s a powerful anti-inflammatory, pro-thyroid, anti-stress hormone that’s necessary for both sexes. It:
Opposes the inflammatory effects of estrogen
Protects the thyroid and supports metabolism
Lowers cortisol and balances mood
Supports ovulation and fertility in women
Enhances insulin sensitivity and reduces water retention
Ray Peat called it the most protective hormone in the body. Progesterone helps bring the body out of stress mode and into a place where it feels safe to repair, reproduce, and thrive.
In women, low progesterone is linked to PMS, miscarriage, endometriosis, fibroids, and insomnia. In men, small doses of progesterone can reduce aromatization of testosterone into estrogen, lower prolactin, and calm the nervous system—without impairing libido or muscle mass.
Pregnenolone: The Master Hormone That Fuels the Whole Cascade
Pregnenolone is the upstream precursor to progesterone, DHEA, testosterone, cortisol, and more. It’s made from cholesterol inside the mitochondria—and when mitochondrial function is suppressed, pregnenolone production tanks.
This leads to a situation where the body can’t make enough downstream hormones—even if you're eating all the right macros. Without pregnenolone, your body keeps recycling stress hormones like cortisol and estrogen because it literally can’t make the protective ones. Energy drops. Metabolism slows. Estrogen dominates.
Supplementing with pregnenolone (when timed correctly and paired with thyroid and carb support) can help refill the body’s hormonal reservoir, restore balance, and ease the nervous system out of chronic stress.
The Role of Light in Hormonal Health
If you’ve been working on your hormones but ignoring your light environment, you’re missing a major pillar of healing. In pro-metabolic frameworks, light is treated as a nutrient—not just a mood booster or sleep aid, but a key activator of hormone synthesis, detoxification, and thyroid function.
Morning and evening sunlight—rich in red and infrared wavelengths—penetrates deep into tissues and stimulates mitochondrial energy production by activating the enzyme cytochrome c oxidase. This increase in ATP production is not just about energy. It’s essential for the conversion of cholesterol into pregnenolone, the starting point of your entire hormonal cascade. No light = no pregnenolone = no progesterone.
Morning sunlight in particular has profound effects on the brain and endocrine system. Within 30 minutes of waking, exposure to natural light—without sunglasses or glass barriers—helps reset your circadian rhythm by activating the suprachiasmatic nucleus (SCN). This regulates pulses of cortisol, thyroid hormone, dopamine, and sex hormones throughout the day. It also helps suppress prolactin, a stress hormone that suppresses ovulation, libido, and testosterone when elevated.
Ray Peat often described this light exposure as a form of “metabolic permission”—a biological signal that it’s safe to shift from stress hormones into reproductive, restorative function.
If you don’t have consistent access to natural light, red light therapy can be used to mimic these mitochondrial benefits. Red and near-infrared LEDs (typically 660 and 850 nm) help stimulate mitochondrial respiration, reduce oxidative stress, and promote hormone synthesis in the thyroid, ovaries, adrenals, and even the brain. Both Peat and Dinkov have emphasized how red light can aid in lowering estrogen, restoring progesterone and testosterone, and improving liver detox function—all without pharmaceuticals.
Equally important is avoiding blue light at night, which delays melatonin production, elevates cortisol, and interferes with estrogen clearance. Your hormonal rhythm depends on the contrast between bright, warming light early in the day, and dim, red-toned light after sunset. Hormone health isn’t just about what you take or eat—it’s about when you’re in darkness, and when you’re in light.
Restoring Balance: Why Bioidentical Support Works Best with Food and Light
Progesterone and pregnenolone can be restored with bioidentical support—but only when the terrain is ready. If you don’t eat enough, if your thyroid is suppressed, or your liver and gut are compromised, simply adding a hormone cream won’t fix the root. In some cases, it can worsen symptoms by pushing the body too fast.
Dr. Mercola has long recommended bioidentical hormone replacement as a safer, more effective alternative to synthetic HRT. Ray Peat and Georgi Dinkov take it further: using low-dose bioidentical support alongside carbohydrate repletion, light therapy, and thyroid support to restore physiologic hormone function, not override it.
This is what I help my clients do: rebuild hormonal balance from the root. We don’t just chase symptoms. We restore energy, unblock detox pathways, rewire light rhythms, and let the hormones follow.
Next Steps
If you’re living with hormone symptoms that just won’t budge—whether it’s PMS, weight gain, low libido, bloating, anxiety, or poor sleep—it’s time to stop guessing. Estrogen dominance is more common than ever, and most people are treating it from the wrong end. It’s not just about estrogen—it’s about the metabolic collapse that lets estrogen take over.
Whether you're male or female, cycling or post-menopausal, I can help you understand what’s going on in your body and how to restore balance—with food, light, and strategic support.
👉 Schedule a one-on-one session on my scheduling page and let’s build your hormone repair plan.
References:
Peat, Ray. “Estrogen, Progesterone, and Cancer: Conflicts of Interest in Regulation and Product Promotion.”
https://raypeat.com/articles/articles/estrogen-progesterone-cancer.shtmlPeat, Ray. “Aging, Estrogen, and Progesterone.”
https://raypeat.com/articles/aging/aging-estrogen-progesterone.shtmlPeat, Ray. “Three Hormones — Progesterone, Pregnenolone & DHEA.”
https://raypeat.com/articles/articles/three-hormones.shtmlDinkov, Georgi. “Progesterone as the Primary Anti-Stress Hormone.”
https://haidut.me/2015/04/04/progesterone-as-anti-stress-hormoneDinkov, Georgi. “Estrogen as a Metabolic Suppressor and Inflammatory Hormone.”
https://haidut.me/2016/02/20/estrogen-metabolic-suppressorFeldman, Jay. “Estrogen Physiology and Why Progesterone Is Protective.”
https://www.jayfeldmanwellness.com/ep-125-wendy-sellens-on-estrogen-what-she-got-wrongMacLean II, J.A., & Hayashi, K. “Progesterone Actions and Resistance in Gynecologic Disorders.” Cells (2022).
https://pubmed.ncbi.nlm.nih.gov/35203298/Prior, Jerilynn C. “Progesterone for Treatment of Perimenopausal Symptoms.”
https://www.cemcor.ca/resources/progesterone-treatmentPrior, Jerilynn C. “Ovulatory Disturbances and Estrogen Excess.”
https://www.cemcor.ca/resources/ovulation-and-estrogen-dominance
Grains: From Gut Damage to Nourishment
Grains Built Civilization—and Broke the Human Body
Grains created civilization. When not properly prepared, they also create chronic disease.
For most of human history, grains were not considered food. Our hunter-gatherer ancestors didn’t wake up and forage for wheat berries. They hunted animals, dug up roots, gathered fruit, cracked open nuts, and moved on. It wasn’t until 10,000 years ago—just a blink in evolutionary time—that humans started eating the seeds of grass: grains.
That shift changed everything. It birthed civilization... and disease.
When humans first domesticated wheat and other grains in the Fertile Crescent, it allowed them to stop being nomadic. They could store calories. Populations grew. Cities formed. But so did malnutrition, stunted growth, infections, and epidemics. The Dark Ages were not a time of robust health. People lived short lives—often only long enough to reproduce—then died of malnourishment, infections, or famine.
Pre-agricultural hunter-gatherers often lived long, robust lives. Once grains took over the food supply, humans started living just long enough to reproduce—then dying of gut damage, infections, and nutritional collapse.
Archaeological records show that skeletal structure, dental health, and immune resilience all declined with the adoption of agriculture. And it wasn’t just the absence of meat—it was the presence of poorly prepared grains, consumed in massive quantities with no understanding of their gut-damaging effects.
Why Grains Wreck the Gut (If You Eat Them Wrong)
Grains contain anti-nutrients—especially in the bran layer (the part that makes it a "whole grain"). These include:
Phytates that bind zinc, iron, calcium, and magnesium
Lectins that irritate the intestinal lining
Enzyme inhibitors that block digestion
Gluten is just one of many gut irritants.
In their raw or unfermented form, grains are harsh. They slow motility, feed pathogens, and create chronic low-grade inflammation. This leads to leaky gut, food sensitivities, and autoimmunity—especially when someone is in low energy availability (LEA), undereating, or malnourished.
Grain proteins aren’t the root cause of autoimmunity—but in a stressed, underfed, or nutrient-deficient body, they absolutely become a trigger.
But Here’s the Truth: Grains Aren’t Evil. They’re Just Unprepared.
Many ancient cultures figured this out.
They didn’t eat brown rice.
They didn’t eat store-bought flour.
They didn’t eat whole wheat sandwich bread.
They fermented, nixtamalized, dehulled, and slow-cooked grains until they became digestible. They paired them with animal foods rich in protein, B vitamins, and fat-soluble nutrients. And they didn’t base their entire diet on them.
Proper grain prep is a lost art in the West—but it’s not gone forever.
The 4 Grains I Recommend (When Your Body is Ready)
Not everyone tolerates grains—especially those still healing their gut or recovering from decades of carb restriction, PUFA overload, or metabolic stress. But for those who have restored their energy availability and built metabolic resilience, these four are typically the most well-tolerated:
1. Sourdough Bread
Every culture that consumed wheat fermented it first. All bread used to be sourdough—even on the American frontier. Laura Ingalls wasn’t eating Wonder Bread. She was using wild yeast and fermentation to break down gluten, phytates, and lectins. Europe still does this in many regions today.
Modern bread? It’s garbage. Commercial flour is bleached, brominated, fortified with synthetic vitamins, and often contains iron filings (yes, actual metal shards). No wonder so many people feel better without it.
But real sourdough made from organic, unbrominated white flour is a completely different food—and in many cases, it’s gut-healing.
Avoid: commercial bread (brominated, bleached, full of synthetic vitamins and metal shavings)
How to Spot Real Sourdough
Most store-bought “sourdough” is a lie. It’s just commercial yeast + vinegar for fake tang. No fermentation. No gut benefits.
What to look for at a bakery or label:
Ask: “Do you use a real sourdough starter?”
Look for: organic, unbleached, unbromated white flour
Avoid: “Whole grain sourdough” (bran = no thanks)
Bonus: Long-fermented (24+ hours = more gluten/phytate breakdown)
Real sourdough should have 3–5 ingredients: flour, water, salt, and sourdough starter. That’s it. If they can't name the starter or it lists yeast, it's not real.
2. White Rice
Not brown. Ancient Asian cultures went to extreme effort to create white rice—pounding or polishing off the bran layer by hand. Why? Because the bran is where all the toxins are. They didn’t do this for fun; they did it because they felt better.
White rice is:
Low-residue
Low-inflammatory
Incredibly easy to digest
It’s ideal in times of healing and pairs beautifully with mineral-rich animal foods and fruit.
Avoid: brown rice (still contains the bran = high in anti-nutrients)
3. Masa Harina (Nixtamalized Corn)
Corn in its natural state is hard to digest. But Indigenous peoples of Mesoamerica developed a brilliant process called nixtamalization—soaking corn in lime (calcium hydroxide) to neutralize anti-nutrients, increase calcium and B vitamin bioavailability, and improve texture.
Masa harina is the result. It’s what tortillas used to be made from before the food industry took shortcuts. When made traditionally, it's a nourishing starch that pairs beautifully with bone broth, cheese, beef, or eggs.
Eat as: tortillas, tamales, pupusas, or mash it with butter and cheese
4. Sprouted, Soaked Oats (Only if Acid-Prepared)
Oats are only tolerable when properly prepared—and that means sprouted and soaked in an acidic medium, like:
Raw buttermilk
Yogurt
Kefir
Water with apple cider vinegar or lemon juice
This neutralizes enzyme inhibitors and phytates that would otherwise block mineral absorption and inflame the gut.
I soak my sprouted oats overnight. Then I slow cook them with mineral-rich water and pair with raw honey, collagen, or fruit.
What to Cook Oats In
If you’re going to eat oats, don’t just soak them—cook them in something mineral-rich. Water alone won’t cut it.
Best cooking mediums:
Raw milk or gently pasteurized whole milk
Milk + water combo for lighter texture
Bone broth if savory
Add collagen, honey, and sea salt to boost mineral profile
Avoid:
Quick oats (they’re overly processed)
Oat milk (PUFA-rich and gut-irritating)
Personally, I slow-cook sprouted oats in raw milk with a pinch of salt, a scoop of collagen, and a swirl of honey or maple. It’s insanely healing.
What About Oatmeal Cookies, Granola, and Baked Goods?
Oats aren’t just for porridge. Some people find they tolerate baked oats better—probably due to slower digestion and better starch transformation from baking.
Safer options:
Oatmeal cookies made with soaked/sprouted oats
Granola made with soaked + dehydrated oats
Oat flour pancakes (if made from sprouted oat flour)
The same rule applies: prep the oat first (soak, sprout, or buy pre-sprouted) and avoid inflammatory add-ins like canola oil or nut butter.
Why the Bran Is the Most Harmful Part of the Grain
We’ve been sold the lie that whole grains are healthier. In reality, the bran layer—the very part that makes a grain “whole”—is the most gut-damaging.
It’s loaded with:
Phytates that bind zinc, iron, calcium, and magnesium
Lectins that irritate the intestinal lining
Enzyme inhibitors that slow digestion
Fibrous grit that mechanically damages the gut wall
Ancient cultures went out of their way to remove or ferment the bran because they understood, intuitively, that this part of the grain made them feel worse. Modern food science is just now catching up—and most of it’s still bought and paid for by industry.
Whole Grains: A Government-Endorsed Lie?
We’ve been brainwashed to believe that “whole grains” are healthier. They aren’t. The outer shell of the grain—the bran—is what ancient cultures worked so hard to remove. It’s loaded with anti-nutrients, not magical fiber.
But the U.S. government, backed by the grain industry and Big Pharma, keeps telling us to eat them. Why?
Cheap grains = higher margins
Chronically inflamed people = more prescriptions
There’s no money in metabolic healing.
There’s no lobby for sourdough.
It’s Not the Grain. It’s the Context.
My partner has ulcerative colitis. When he ditched commercial bread, his symptoms dropped by 80%. Today, he eats sourdough every day—with no flare-ups.
Why? Because he’s eating it in the context of a high-calorie, high-carb, low-fat, nutrient-rich diet with plenty of collagen, dairy, and cooked vegetables.
Grains aren’t evil. But they’re not innocent either.
To tolerate them well:
Heal your metabolism
Exit low energy availability
Lower your fat intake (especially seed oils)
Get your body temperature and thyroid up
Then slowly reintroduce one properly prepared grain at a time
Grains Aren’t Evil. Just Unprepared.
Ditch:
Brown rice
Whole wheat
Commercial bread
Quick oats
Unfermented grains
Consider (when ready):
Heal your gut. Exit LEA. Then reintroduce ancient wisdom.
Cold Plunges, Cortisol, and Carnivore: The Biohacked Burnout of Carb Deficiency
You don’t have adrenal fatigue. You have a glucose deficiency.
I just listened to the Joe Rogan x Gary Brecka interview from a few months ago, and by the end of it, I felt like I was eavesdropping on two men trying to survive a famine — one cold plunge and ozone sauna at a time.
No one said the word “cortisol” once. Not in a 2.5-hour conversation about stress, optimization, morning routines, energy crashes, and biohacking.
Not. One. Time.
But that’s exactly what this was: a full-length, high-production podcast episode on how to manually override your biology when your body is running on stress hormones 24/7 because you refuse to eat a carbohydrate.
The Carnivore Grind: Steak for Breakfast, Stress for Dessert
You know the type.
Shawn Baker, Anthony Chaffee, Ken Berry — the poster boys of "peak performance" on a diet of nothing but ribeyes, butter, and beef liver.
No carbs. No sugar. No fruit.
But plenty of cortisol.
Let me say it plainly: these men are not thriving.
They are surviving — on adrenaline, norepinephrine, and every biohack under the sun.
You see them chugging coffee, skipping meals, hitting the cold plunge at 5am, blasting red light at their faces, popping testosterone injections, taking metformin “for longevity,” meditating while wired and inflamed, bragging about how they haven’t had a carb since 2003...
That’s not health. That’s crisis management.
Cold Plunges Are a Symptom, Not a Solution
Don’t get me wrong — I love a good cold plunge. But let’s be honest about what it is:
It’s a sympathetic nervous system bomb.
If you need a freezing tub of water, followed by coffee, followed by red light therapy, just to feel alive — you're not optimizing. You're desperately chasing the dopamine your nervous system is too depleted to produce.
And if you’ve been living in ketosis long enough, that might be the only way to feel anything at all.
Cortisol Is Carrying You (and You’re Calling It Discipline)
Carbohydrate deficiency triggers a predictable cascade:
Liver glycogen tanks.
Blood sugar drops.
The body panics.
Adrenal glands crank out cortisol to keep you conscious.
At first, you feel “clear-headed,” “sharp,” maybe even “unstoppable.”
Because cortisol feels good — for a while.
Until it doesn’t.
Eventually you crash:
Insomnia
Constipation
Blood sugar swings
Anxiety
Tanked testosterone
Fatigue so deep it takes an ozone chamber and 16 supplements just to take a poop
This isn’t vitality. It’s just living off your stress hormones.
The Truth About Carnivore "Optimization"
Let’s talk about the carnivore influencers.
A recent comment from Jay Feldman or Mike Fave (I forget which, they both crush) mentioned that Shawn Baker’s testosterone is allegedly bottomed out. Like… dangerously low.
How does that happen to a guy who lifts every day and eats nothing but steak?
Simple: no carbs = no insulin = no conversion of thyroid hormone = no signal to the testes = no testosterone.
Yes, you can look shredded while running on fumes.
Yes, you can build muscle while slowly tanking your metabolism, hormone function, and mental health.
But you won’t feel good. And it won’t last.
I Was There Too
I’m not writing this from the outside. I lived it.
I was keto for eight years — hardcore. The last year of that, I went full carnivore. I hadn’t eaten more than 20 grams of carbs a day in nearly a decade. I lived off ribeyes and coffee, and listened religiously to every podcast Paul Saladino put out.
And then, one day, I heard him talking about the dangers of long-term carb restriction — and it hit me like a truck. Every symptom he described? I had it:
Muscle cramping
Morning anxiety
Insomnia
Low libido
Cold hands and feet
PMS from hell
Joint pain
Depression
Constipation
Eventually I tested my thyroid and found out my T3 was low — the missing puzzle piece that made everything make sense. I was stuck in survival mode, living off cortisol, pretending it was “discipline.”
So I did something radical:
I added back carbohydrates. Not all at once, but in small, steady amounts, spaced throughout the day. Within weeks, every single symptom started to disappear. My mood stabilized. I could sleep. My cycle regulated. My body warmed up. I came back to life.
Carbs Are Not the Enemy — They’re the Missing Piece
Carbs are not toxic.
Sugar does not “feed disease.”
Fruit is not why you’re tired.
You’re tired because your mitochondria haven’t seen glucose since Obama was in office.
Carbohydrates are:
The body’s preferred fuel
The thyroid’s best friend
The antidote to cortisol
The fuel for progesterone, serotonin, dopamine, and testosterone
You don’t need another cold plunge.
You need orange juice.
Summary — The Biohacked Burnout Checklist
Cold plunges are a cortisol crutch
Carnivore = constant stress signal
Low-carb = low testosterone, low thyroid, low mood
Biohacking is just symptom suppression in disguise
Real energy starts with eating carbs — not avoiding them
Final Thought
If you need an elaborate “morning routine” to feel functional… you’re probably missing the most basic routine of all:
Eat carbs. Often. Especially in the morning.
You don’t need 10 supplements, 3 gadgets, and a neurofeedback helmet.
You need glucose.
Sip Your Way to Stable Blood Sugar
Why Drinking Protein + Carb Mini Meals Works
Small sips, big impact. Support your thyroid, lower stress hormones, and hit your macros without bloating.
For years, mainstream nutrition pushed three square meals a day—or worse, fasting windows and long gaps between meals—as the gold standard for “metabolic health.” But if you’re healing your metabolism, restoring energy availability, or trying to lose fat without tanking your thyroid, there’s a better way. And it might be hiding in your blender.
Enter: liquid protein + carb mini meals, spaced throughout the day.
We’re talking 6 small meals every 2–3 hours, mostly drank—not chewed. Think orange juice and collagen, skim milk and honey, smoothies with fruit and nonfat Greek yogurt. These aren’t meal replacements. They’re strategic tools to keep your metabolism humming, blood sugar stable, and stress hormones low—especially during a cut or a healing phase.
Why It Works: Blood Sugar, Cortisol, and Energy Efficiency
Eating small, frequent meals that combine protein + carbs:
Prevents blood sugar crashes
Stable glucose = stable mood, fewer cravings, and better willpower.
Blunts cortisol spikes
Every time you go too long without food, cortisol kicks in to raise blood sugar via gluconeogenesis. That’s muscle-wasting, thyroid-suppressing, and metabolism-slowing. No thanks.
Supports the thyroid
Your thyroid needs sugar and aminos throughout the day to produce T3 and keep your temps up.
Boosts digestion
Liquid meals are gentler on the gut. For anyone healing from SIBO, IMO, or low stomach acid, they’re easier to digest and absorb—especially when fiber is temporarily reduced.
Spreads out your macros
You can hit your targets (especially high carb + low fat) without bloating or overwhelming your system in one sitting.
Metabolic Benefits on Tap
This isn’t about grazing or snacking. These sippers are metabolically strategic mini meals designed to:
Protect lean muscle
Stabilize blood sugar
Keep your liver and thyroid fueled
Maintain mood, energy, and focus
Hit macro targets (especially during a cut or reverse diet)
Who Benefits Most?
Anyone in a cut
Fewer calories = less room to feel full. Drinking your meals makes it easier to avoid hunger while still packing in nutrients.
People recovering from LEA (low energy availability)
Small meals reduce the burden on digestion and keep fuel flowing to the cells.
Anyone with poor appetite or hypoglycemia
Liquid meals go down easier and stop the blood sugar rollercoaster.
Athletes and busy professionals
No cooking, no cleanup. Shake it and sip.
What to Drink: Meal Ideas
High-carb, low-fat, bloat-free & metabolism-friendly
Use these between whole-food meals to hit your macros, or build your entire day around them if you're in a deep cut or digestive flare.
Orange Julius Smoothie
6 oz orange juice
1/2 cup nonfat Greek yogurt
2 tbsp collagen
Splash vanilla extract
~22g protein, 32g carbs, 0g fat
Maple Milk
1 cup skim milk
2 tbsp collagen
1 tbsp maple syrup
Dash vanilla + pinch salt
~22g protein, 25g carbs, 0g fat
Maple Collagen Latte
1 cup strong brewed coffee or 2 shots espresso
1 cup skim milk
1 tbsp maple syrup
2 tbsp collagen
~22g protein, 25g carbs, 0g fat
Blend or froth for that creamy café vibe—perfect pre-walk or AM blood sugar support.
Metabolic Chocolate Milk
1 cup skim milk
2 tbsp collagen
1 tsp unsweetened cocoa
1 tsp honey
~20g protein, 20g carbs, 1g fat
Strawberry Yogurt Shake
1/2 cup nonfat Greek yogurt
1/4 cup strawberry lemonade
2 tbsp collagen
Splash water or coconut water to thin
~25g protein, 20g carbs, 0g fat
Tropical Glow Smoothie
1/2 cup pineapple juice
1/2 cup frozen mango
1/2 cup nonfat Greek yogurt
2 tbsp collagen
Squeeze of lime + pinch salt
~22g protein, 32g carbs, 0g fat
Peaches & Cream Sipper
1/2 cup canned or stewed peaches (in juice, drained)
1/2 cup lowfat cottage cheese or nonfat Greek yogurt
1 tbsp maple syrup or honey
Dash cinnamon (optional)
Splash of water or almond milk to thin
~22g protein, 28g carbs, 1–2g fat
Carrot Cake Elixir
1/2 cup carrot juice
1/2 cup skim milk
2 tbsp collagen
1 tbsp maple syrup
Dash cinnamon + pinch salt
~22g protein, 28g carbs, 0g fat
Fat Loss Without the Stress
When you're in a fat loss phase (or just trying to maintain muscle while trimming down), the biggest enemy isn’t calories—it’s stress. Frequent protein + carb meals are your anti-stress armor. They prevent the body from shifting into catabolic mode, where it burns muscle, lowers thyroid, and stores fat out of survival.
A stable metabolism is a flexible one—one that trusts it will be fed consistently and doesn’t panic. That’s how you lose fat without the insomnia, hair loss, fatigue, or rebound.
Why Sip Mini Meals?
✔ Easier to digest
✔ Blunts hunger and cortisol
✔ Keeps blood sugar stable
✔ Helps hit high-carb/low-fat targets
✔ Protects thyroid, muscle, and mood
✔ Keeps energy steady during healing or a cut
Whether you’re deep in a cut or climbing out of burnout, sipping your meals might be the metabolic magic trick you were missing.
Why Gut Issues Often Return During a Cut
If you’re finishing a fat loss phase and suddenly feel like your digestion is worse—bloating, gas, constipation, food sensitivities flaring up—you’re not crazy. But let’s be very clear: this is not a sign that carbs are the problem. It’s a sign that your gut—and your entire body—is still in a malnourished state.
I see this all the time with clients. They’ve been cutting for 4–6 weeks, running on lowered energy availability, and the minute we start refeeding or adding carbohydrates back in, gut issues resurface. Their first instinct? “The carbs are causing it.” I hear the panic:
“It must be the sourdough.”
“I’m feeding candida again.”
“I think I need to go back to keto.”
No. Let’s break this down.
Cutting Starves the Gut—Literally
A cut isn’t just a reduction in energy. It’s a drop in micronutrients, fiber, fermentable substrates, and metabolic signals like T3. It’s a famine state. And guess who else goes hungry?
Your gut bacteria.
During a cut, your beneficial microbes—the ones that keep pathogens in check and maintain the gut lining—get underfed. And when that happens, two things start to unravel:
The mucosal barrier thins.
The immune system downregulates.
Digestion slows down—because the body shunts energy toward more essential systems like the brain, heart, and muscles, leaving less fuel for enzyme production, bile flow, and peristalsis.
This creates an opening for pathogenic or opportunistic microbes to sneak in or re-establish dominance. So when you reintroduce carbs—especially fermentable ones—you might feel worse not because you’re feeding the “bad bugs,” but because you’re finally feeding the good ones, and they’re trying to reclaim territory.
That process? It’s called die-off. Or more accurately: a Herxheimer reaction.
Die-Off ≠ Overgrowth
Die-off symptoms—fatigue, mood swings, bloating, skin flares, weird body odor, changes in bowel movements—often mimic what people assume are “overgrowth” symptoms. But this isn’t a sign of fungal relapse or bacterial disaster. It’s a war. And the good guys are winning.
When you increase carbohydrates, especially after a long period of underfeeding, you:
Reawaken dormant digestive fire (T3 rises)
Stimulate bile and enzyme production
Feed SCFA-producing bacteria (SCFA = short-chain fatty acids, like butyrate and acetate, which strengthen the gut lining, reduce inflammation, and improve motility)
Starve out methane-producing archaea and sulfate-reducing bacteria by increasing gut movement
Yes, this process is uncomfortable. But it is necessary for long-term gut repair.
Not All Carbs Are Created Equal (Especially After a Cut)
A huge mistake I see? Clients try to reintroduce the same types of carbs they thrived on at maintenance—sourdough, white rice, salads, berries with seeds, potato skins, cassava, even sprouted oats or whole fruits with lots of fiber. But post-cut digestion is fragile. T3 is still suppressed, enzyme output is low, and motility is sluggish.
What digests well at maintenance might wreck you during refeed.
This is not a sign that you’re broken. It’s a sign to shift strategy.
The Best Carbs for Gut Repair (Refeed Edition)
Your digestion during a refeed is not “normal.” It is compromised, sluggish, and healing. Here’s how to approach carbs during this fragile but critical rebuilding window:
Stick to the easiest-to-digest carbs:
Liquid carbs: fruit juice, coconut water, organic lemonade, Italian soda (cane sugar), kombucha (if tolerated), honey, maple syrup, and skim milk (raw is best)
Whole fruits that have low fiber and seeds: mango, melons, stone fruit like peach and plum
Cooked, peeled tubers like sweet potato or white potato (only if well tolerated)
Fiber carbs must be well tolerated. Avoid if they cause symptoms:
Sourdough (even well-fermented)
White rice (especially for those with methane archaea or IMO)
Berries with seeds
Potato skins
Sprouted oats
Raw salads
Cassava
Any raw or undercooked fibrous vegetables
Your gut may handle these better after 2–4 weeks of consistent refeeding with easier carbs.
Important: Everyone digests carbs differently.
Your ability to digest carbohydrates depends on your bacterial diversity, enzyme output, and even stress levels. What works for one person (white rice, sourdough, beans) may not work for another. I always recommend starting with the simplest carbs and slowly layering in fiber once symptoms stabilize and metabolic markers (like body temp and motility) improve.
The Mental Trap: Blaming Carbs
Most of us have internalized decades of carb-phobia. So when digestion goes haywire, it’s easy to fall back on the belief that carbs are to blame. But let me say this bluntly:
It’s not the carbs. It’s the malnourishment.
Carbs didn’t cause your weight gain. Swampland did (that high-fat/high-carb no man’s land where nothing burns efficiently).
Carbs aren’t triggering your yeast. They’re triggering your immune system to respond as your gut terrain shifts.
If anything, the cut—especially one done with moderate to high fat—is what destabilized your microbiome in the first place.
The Refeed Feels Worse Than the Cut (And That’s Normal)
Most people expect to feel better when refeeding. More food = better, right?
Not always.
Early refeed can be even harder than the cut itself, because your body is still downregulated:
Metabolism is low (T3 takes time to rebound)
Digestion is weak (enzymes are sluggish)
Detox pathways are backed up (no bile, poor methylation)
Gut bugs are fighting for dominance
You’re still technically in a malnourished state. But now you’re introducing fermentable fuel. This combo can trigger temporary chaos.
The key? Push through—gently. Don’t overdo fiber. Don’t crank fat back up. Stick to simple carbs and digestible foods. Trust the process. You’re rebuilding.
My Pro-Metabolic Refeed Rules for Gut Repair:
Keep fat ultra-low during early refeed (0.3–0.4 g/kg)
Use simple, low-residue carbs (fruit juice, maple syrup, coconut water, Italian soda)
Split carbs across 4–5 meals/day for blood sugar and motility
Support detox with daily raw carrot or bamboo shoots
Temporarily avoid high-fiber carbs unless well tolerated (sourdough, berries with seeds, sprouted grains, etc.)
Gradually layer in cooked, peeled tubers only if tolerated
Track symptoms and metabolic markers (temps, pulses, stools)
Don’t fear a little bloat or gas—it’s part of the rebuild
Summary:
Gut issues after a cut aren’t because of carbs—they’re because of the cut.
Carbs feed beneficial bacteria that repair the gut lining and outcompete pathogens.
The refeed can trigger die-off, not overgrowth—don’t confuse the two.
Your digestion is compromised post-cut, even for foods you normally tolerate.
Stay low-fat, stick to easy carbs, and allow time to heal.
And most importantly: your gut needs nourishment, not another restriction cycle.
Jaggery: The Forgotten Sweetener That Actually Nourishes You
When most people talk about sugar, it's either demonized as the root of all evil or worshipped in its raw, crunchy, coconut form. But somewhere between the extremes of white sugar and bitter blackstrap molasses, there’s a forgotten hero of mineral-rich sweetness: jaggery.
Never heard of it? You’re not alone. But if you’ve been chasing the pro-metabolic life and want a sweetener that actually does something for your body, jaggery deserves a place in your pantry.
So… What Is Jaggery?
Jaggery is an unrefined sugar made by boiling down sugarcane juice (or occasionally date palm sap) into a thick, sticky, mineral-rich paste that’s dried and molded into blocks or powder. The key difference?
The molasses stays.
That means jaggery contains both the sugar and the minerals in one whole-food package.
Unlike white sugar, which is stripped, bleached, and purified into pure sucrose — and unlike brown sugar, which is basically white sugar with a little molasses added back in as an afterthought — jaggery is the real deal. It’s how sugar used to be.
Nutritional Breakdown
Per tablespoon, jaggery offers a surprising dose of:
Iron (especially useful if you're healing from anemia or menstruating)
Calcium + Magnesium (mineral support for bones, thyroid, and adrenals)
Potassium (key for hydration, insulin sensitivity, and blood sugar stability)
B Vitamins (small amounts of B6, B2, B1)
Still a sugar? Yes. But it’s a sugar your body recognizes — not just a calorie bomb with nothing to offer.
Pro-Metabolic Uses
Jaggery isn’t just a sweetener — it’s a functional food. I recommend it to clients who:
Are healing from low iron or adrenal fatigue
Want a whole-food source of sweetness with actual value
Need a pre-workout glucose bump without the crash
Are transitioning off refined sugars or artificial sweeteners
Want to improve insulin sensitivity without overloading on pure sucrose
Favorite ways to use it:
Stir into tea or coffee (just like honey)
Add to warm milk with collagen for a mineral-rich bedtime treat
Use in energy balls with gelatin and coconut flour
Melt into oatmeal or mashed sweet potatoes
Mix with ghee for a traditional Ayurvedic immune booster
What to Watch For
Some jaggery on the market is adulterated with white sugar or made in unsanitary conditions. Look for:
Certified organic or traditional handmade jaggery
Ingredients: 100% cane juice or date palm sap
Block, paste, or powder form with no additives
Summary
Jaggery = whole cane sugar + molasses + minerals. Unlike white sugar, it feeds your cells — not just your cravings. It’s rich in iron, potassium, magnesium, and B vitamins. Use it in moderation like you would honey or maple syrup, but know you’re actually supporting metabolism with every bite.
Real Sweeteners Do Real Things
In the pro-metabolic world, we don’t fear sugar — we respect it. The type of sugar matters. If you’re still spooning white sugar into your coffee or pretending brown sugar is “less bad,” it might be time to meet jaggery.
She’s ancient, mineral-rich, and here to nourish your cells — not rob them.
What Did Hunter-Gatherers Really Eat?
Spoiler: It Wasn’t Grains, Almonds, or Bacon
For decades, the public has been sold a fantasy version of the “paleo diet.” Flip through a popular paleo cookbook and you’ll see heaping plates of ribeyes, piles of nuts, and endless “grain-free” breads made with almond flour. This glossy picture has almost nothing to do with what our ancestors actually ate. If you want the truth about human metabolism and ancestral nutrition, you have to step away from modern reconstructions and look at the real evidence from living hunter-gatherers, primate biology, and archaeology. The reality is both surprising and liberating: our ancestors weren’t keto, and they weren’t scarfing down handfuls of almonds. They were carb-powered primates who lived on honey, fruit, roots, and modest amounts of animal food—with very little fat.
Grains and Nuts: Modern Myths About Ancient Foods
Let’s start with what they didn’t eat. The idea that hunter-gatherers survived on wild grains is mostly projection. Wild grains existed, but they were small, bitter, and packed with antinutrients. They required extensive processing—pounding, grinding, soaking—to yield meaningful calories. Grinding stones have been found in the archaeological record, but this proves only that early humans could process grains, not that they were staples. At best, grains were fallback foods in times of scarcity, not everyday fare. Agriculture only made grains truly accessible by breeding them into larger, sweeter, less toxic varieties.
Nuts are another modern misconception. Today’s almonds, walnuts, and cashews are heavily domesticated, bred to be palatable and high-yield. Wild versions were often bitter and sometimes toxic. While some groups consumed nuts like mongongo or acorns, they did so seasonally and only after elaborate detoxification steps like soaking or leaching. They were never daily staples, and they certainly weren’t the PUFA-laden snacks that line modern supermarket shelves. To imagine the Hadza walking around with almond milk lattes is pure fantasy.
The Real Building Blocks of the Human Diet
So if not grains and nuts, what did hunter-gatherers rely on? Ethnographic evidence, especially from the Hadza of Tanzania, paints a very different picture. Their diet revolves around five food categories: honey, fruit, tubers, baobab, and meat. Of these, honey and tubers are particularly central. Honey is the single most prized food of the Hadza, sometimes making up 15–20 percent of total calories. Men will climb dangerous heights to raid hives, bringing back combs dripping with sugar and bee larvae. Tubers, on the other hand, are the fallback food—the reliable starch that sustains the group through lean seasons.
Fruit and berries round out their plant staples. These wild fruits are not the oversized candy bombs you find in today’s grocery stores; they are smaller, denser, and typically higher in protein and minerals. Baobab fruit pulp and seeds provide important minerals, with the seeds being one of the few significant fat sources in the Hadza diet. Meat does play a role, but it is irregular and opportunistic—sometimes abundant, sometimes absent for days. And even when consumed, much of the meat is lean.
Taken together, the Hadza diet is overwhelmingly carbohydrate-based, with roughly two-thirds of energy coming from starches and sugars, around 15–20 percent from protein, and only about 10–15 percent from fat. This matches estimates from other indigenous groups like the Kitavans of Papua New Guinea, whose diet is nearly 70 percent carbohydrates from tubers and fruit, with very little fat. It’s also strikingly similar to the Okinawan diet—85 percent carbohydrate, mostly from sweet potatoes—which produced some of the longest-lived people on earth.
Humans Are Carbohydrate-Burning Primates
The deeper reason for this macronutrient pattern is evolutionary. Humans are primates, and primates are frugivores. In the wild, fruits make up the bulk of the diet for many monkeys and apes. Studies of wild fruit composition show that they are low in fat—on the order of just five percent by dry weight—while being rich in carbohydrates and fiber. Even chimpanzees, our closest relatives, consume meat in tiny amounts, often less than two percent of total calories. Our digestive systems, teeth, and metabolism all reflect this frugivorous heritage.
In fact, what sets humans apart is not that we abandoned fruit and starches, but that we learned to cook tubers and roots, unlocking massive amounts of digestible carbohydrate. Richard Wrangham, the primatologist who pioneered the “cooking hypothesis,” has shown that the ability to process starches with heat may have been the critical turning point in human brain evolution. Carbs, not fat, powered the expansion of our energy-hungry brains.
The Danger of the “Swampland” Diet
If ancestral diets were so carb-heavy, how did fat become glorified in the modern paleo and keto movements? The confusion stems from conflating occasional fat-rich foods (like baobab seeds or fatty game meat) with the foundation of the diet. In truth, most hunter-gatherers consumed fat sparingly. When you look across cultures—from the Hadza to the Kitavans to the Okinawans—fat intake hovers around 10 to 20 percent of calories, rarely more.
Contrast this with the modern American diet, which is roughly 40 percent fat—half of it from industrial seed oils that were never part of our evolutionary environment. When fat is layered on top of abundant carbs, you get the “metabolic swampland”: a dangerous mix that drives insulin resistance, obesity, and chronic disease. Our ancestors never lived in this swampland. Their diets were either carb-based and low in fat, or in rare cases, fat-based and seasonal (such as Inuit relying on blubber during certain times of the year). But never both at once, and never with seed oils.
Carbs as Metabolic Medicine
The implications for modern health are profound. Carbohydrates are not the enemy—they are essential for thyroid function, sex hormone balance, and metabolic rate. The conversion of T4 to active T3, the hormone that sets metabolic speed, depends on glucose availability. Progesterone production also requires adequate carbohydrate supply, which is why carb restriction often disrupts menstrual cycles. Even body temperature, a reliable marker of metabolic health, drops when carbs are insufficient.
This explains why people transitioning to pro-metabolic, high-carb, low-fat diets often feel warmer, more energetic, and hormonally balanced. It also explains why groups like the Hadza, Kitavans, and Okinawans remain lean and free of chronic disease despite consuming far more sugar and starch than the average American dares to imagine. The difference is not the presence of carbs but the absence of excessive fat, especially polyunsaturated fat.
Rethinking “Paleo”
So what did hunter-gatherers really eat? They ate honey, fruit, roots, lean meat, and the occasional fatty seed or animal organ. They did not eat large quantities of grains, nuts, or dairy. They did not eat seed oils, processed foods, or butter-drenched ribeyes. Most importantly, they did not eat high-fat, high-carb hybrid diets that suffocate the metabolism.
Our true ancestral blueprint is high-carb, moderate-protein, and low-fat. It is the diet of primates, the diet of the Hadza, the diet of the Kitavans and Okinawans, and the diet that keeps the thyroid and metabolism humming. Carbs are not just safe—they are essential. And the sooner we stop fearing sugar and start respecting the frugivorous design of our species, the sooner we can reclaim the metabolic resilience our ancestors enjoyed.
References
https://pubmed.ncbi.nlm.nih.gov/19350623/
https://anthropology.ucsd.edu/_files/Faculty%20Files/schoeninger-publications/Murray%20etal.2001.pdf
https://sciencebasedmedicine.org/what-can-we-learn-from-the-kitavans/
https://stanmed.stanford.edu/hunter-gatherer-diets-offer-clues-to-gut-bug-diversity
Carbs Don’t Cause Insulin Resistance — Dietary Fat Does
Why cutting carbs doesn’t fix the root cause — and why sugar is part of the solution
Obesity, type 2 diabetes, heart disease, and even Alzheimer’s are often packaged under the umbrella of Metabolic Syndrome—a cluster of symptoms unified by one core dysfunction: insulin resistance.
Most clinicians and nutrition ideologies still charge that carbohydrates (especially sugar) are the villains and that eliminating them cures insulin resistance. That narrative is seductive but also misleading—and has likely hurt more people than helped.
From a pro-metabolic framing, insulin resistance isn’t caused by eating too many carbs. It’s caused by your body’s inability to use them properly. That’s a huge distinction—and alters the solution entirely.
Sugar (Carbohydrate) as a Healing Fuel, Not the Enemy
I want to be crystal clear: sugar is not inherently toxic when used in the right context. In fact, in many metabolic healing protocols (e.g. the Ray Peat model), sugar—including from ripe fruit, honey, and even sucrose—is considered one of the most metabolically supportive fuels. The Hadza (an existing primitive society in Tanzania) drink large amounts of honey everyday and have no diabetes.
Key roles sugar (glucose/fructose) plays:
Preferred fuel for liver, brain, and thyroid
Essential for replenishing glycogen in liver and muscle
Potent at lowering cortisol when consumed appropriately
Needed (in many models) for converting T4 → T3
Prevents chronic stress signals by reducing need for gluconeogenesis
Thus the logic: sugar doesn’t trigger insulin resistance—a broken metabolism does.
So why does sugar get blamed? Because almost everyone who suffers from insulin resistance is already operating in a state of metabolic suppression: under-eating, chronic stress, micronutrient deficiency, and chronic exposure to lipid toxins (especially PUFAs / seed oils). Sugar is judged in a body already damaged.
What Actually Drives Insulin Resistance
Here’s a refined list (with emphasis) of what I see as primary causal drivers:
PUFA / seed-oil accumulation in tissues
Seed oils (linoleic, linolenic acids) physically embed into mitochondrial membranes, disrupt electron transport, induce lipid peroxidation, and diminish glucose uptake.Excess dietary fat (especially PUFA) load
In ancestral diets, total fat was often low (~10 % of calories). In modern Western diets, fat has ballooned—often 30–40+ %, heavily from PUFAs. The excess free fatty acids interfere with insulin signaling (Randle cycle).Cortisol / catecholamine dominance
Chronic stress (psychological, environmental, or physiological) favors lipolysis, mobilizing fatty acids and impairing glucose uptake.Low thyroid / low metabolic drive
When your metabolic thermostat is turned down, you burn fewer carbs, producing stagnation in glucose utilization.Micronutrient deficiencies (Mg, K, B1, B3)
These are cofactors in glycolysis, Krebs cycle, pentose phosphate, etc. Without them, glucose metabolism bottlenecks.Undereating / substrate starvation (especially of carbs)
If you chronically restrict carbohydrate intake, you force the body into fat oxidation mode, reduce insulin signaling capacity, and further exacerbate metabolic inflexibility.Mitochondrial / oxidative damage
When mitochondria are oxidatively damaged (often via lipid peroxides from PUFAs), their ability to use glucose is crippled.
When your cells are overwhelmed with fatty acids and oxidative stress, they lose their ability to properly respond to insulin. Glucose uptake fails. Insulin levels rise. Over time, receptor resistance emerges. The solution isn’t to eliminate glucose—it’s to restore the cell’s ability to use it.
Muscle Is the Crucible of Glucose Burning (and Healing)
Skeletal muscle is usually the first tissue to lose insulin sensitivity. That matters, because muscle is the body’s primary sink for glucose disposal. If your muscles won’t take glucose, it gets shunted to adipose tissue or stays in circulation.
Low-carb, high-fat diets tend to worsen this: lower thyroid, higher cortisol, suppressed insulin sensitivity, and high intramuscular lipid deposition (IMCL) that blocks glucose flux (again, the Randle cycle).
So the more muscle you have (or improve in function), the better your capacity to burn sugar—and, ultimately, reduce insulin load.
Swampland Metabolism: What Breaks Your System
I like to think of a “healthy metabolism” as a well-running machine. But many people live in a swampy metabolic state—where nutrients stagnate, gradients flatten, signals get crossed. Swampland is when the body is inundated with large amounts of two different fuels: carbs and fat. What else causes this swamp?
PUFA infiltration in membranes
Low mitochondrial reserve
Chronic stress
Low energy flux (low fuel input, low output)
Toxin burden, inflammation, gut dysbiosis
Maladaptive hormonal loops
Once metabolism is in swamp mode, even “safe” foods get misprocessed. The trick to healing is to drain the swamp—restore mitochondrial energy pathways.
How to Actually Reverse Insulin Resistance (Not Just Mask It)
If insulin resistance is a wound, sugar is a tool, not a weapon. The healing process requires:
Adequate caloric intake
Chronic undereating suppresses thyroid, lowers metabolic rate, and elevates cortisol. Many people reversing metabolism—especially women—require 2,000–2,500+ kcal/day (or more, individual) with 50–60 % carbs (or more) during rehabilitation.Low fat, at least during healing
This doesn’t mean zero fat, but keep fat modest while reconditioning insulin sensitivity. For many, fat levels are capped at ~10–15 % of total calories. Focus on saturated fats (coconut oil, dairy fat, butter) in moderated amounts.Pro-metabolic carbohydrates
Favor easy-to-digest carbs: ripe fruit, fruit juice + protein, honey, root vegetables, dairy sugars. Avoid combining high fat + high sugar in the rehealing phase.Target muscle load & movement
Resistive training 2× weekly, combined with daily walking (8–10k steps), primes glucose uptake machinery (i.e. GLUT4). Over time, the more active your tissues, the more carb capacity you regain.Sunlight / circadian support
Morning sun, proper light exposure, regulated sleep help regulate thyroid, cortisol, and mitochondrial signaling.Restorative sleep & cortisol modulation
Use gentle carb + protein bedtime snacks to lower overnight cortisol surges (e.g. warm milk + honey, cottage cheese + jam).Micronutrient support
Ensure adequate magnesium, potassium, sodium, thiamine (B1), niacinamide (B3), etc. In cases of chronic depletion, short-term supplementation may be warranted.PUFA detox / fatty burden reduction
Over time, reduce dietary PUFAs, seed oils, and encourage cycles (fasting, liver support) that help mobilize and clear stored lipid toxins.Avoiding high-fat, re-feeding spikes too early
Be cautious: reintroducing large amounts of fat while metabolism is still fragile often backfires—pulling the system back into swamp mode.
Over time, insulin sensitivity recovers, glucose becomes a safe and useful fuel again, and you start to reclaim metabolic flexibility.
What About Fructose, Fatty Liver, and The “Fat + Sugar” Myth?
Fructose is demonized, but context is everything. When taken in isolation or in a low-fat matrix (fruit, honey with protein), it is typically shunted into glycogen storage (in liver) rather than lipogenesis. In fact, it’s often repackaged as fuel for vital tissues (thyroid, brain, adrenals). The danger arises when fructose is consumed alongside excess dietary fat, especially PUFAs (think: soda + french fries). That mash-up drives lipogenesis and triglyceride elevation—because the liver is overloaded, and fat export pathways are saturated.
So fruit and honey aren’t the enemy—they become part of the repair toolkit, especially when the metabolic swamp is drained.
Final Takeaway
Insulin resistance is not a carbohydrate problem - it’s a metabolic dysfunction problem. Carbs (and sugars) are not the root of the disease—they’re tools for recovery when wielded strategically.
Healing insulin resistance demands reclaiming metabolic capacity - not by fear, but by fuel, flow, and function. Eat enough. Choose carb-forward, low-fat meals. Move your muscles. Fix your sleep, hormones, and mitochondria. Ditch the fear. Heal the terrain.
Once metabolism is healed, you’ll thrive.
References
Sommerfeld, D. et al. Modern Perspective of the Rice Diet for Hypertension and Metabolic Diseases — Historical and clinical overview of Kempner’s Rice Diet and its metabolic impact.
“The Rice Diet and Duke University.” North Carolina Department of Natural and Cultural Resources — Background on Kempner’s work and the Rice Diet’s outcomes.
Kempner, W. Treatment of Massive Obesity With Rice/Reduction Diet Program. JAMA Internal Medicine (1975) — Clinical data on weight loss and insulin normalization using a low-fat, high-carb rice diet.
Scientific Publications of Walter Kempner, M.D. Vol. 2 — Duke University Archives (PDF) — Comprehensive collection of Kempner’s original studies.
“Can the Rice Diet Reverse Type 2 Diabetes?” NutritionFacts.org — Modern review of Kempner’s diet and glucose metabolism outcomes.
Minger, D. “The New USDA Dietary Guidelines: What the USDA Forgot to Mention.” Raw Food SOS (2011) — Denise Minger’s critique of mainstream nutrition science and misinterpretation of carbs vs. fats.
Minger, D. “Industrial Seed Oils: A Hidden Metabolic Disaster.” Raw Food SOS — Discussion of PUFA oxidation, mitochondrial dysfunction, and insulin resistance.
Mercola, J. “Why You Should Limit Unhealthy Fats, Not Healthy Carbs.” Mercola.com (2023) — Overview of emerging evidence connecting excess fat intake with insulin resistance.
“Insulin Sensitivity and Dietary Fat.” Mastering Diabetes — Mechanistic breakdown of how fat intake modulates insulin response in muscle and liver tissue.
“Seed Oil Misinformation.” Wikipedia — Summary of the public debate on PUFA safety, included for balanced context.
90% of Americans Are Undereating—And Reverse Dieting Is the Metabolic Fix
Learn to eat like your grandparents ate, and heal your body.
Undereating Is Silently Destroying Metabolism, Hormones, Digestion, and Mood—This Is the Strategy to Reverse It.
Reverse dieting isn’t just for bodybuilders coming off a cut or athletes trying to restore energy. It’s the unifying strategy that connects eating disorder recovery, RED-S (Relative Energy Deficiency in Sport), and the slow metabolism that plagues most of the population after years of under-eating. That includes not only classic calorie restriction but also extreme restriction of entire macronutrients. Low-carb, keto, and carnivore diets may seem therapeutic at first, but they often function as socially acceptable eating disorders. These diets can lead to significant energy deficits, hormonal suppression, and impaired metabolic function—especially when combined with intense exercise.
Whether you're coming from years of low-calorie dieting, a history of anorexia or orthorexia, or even just a hard training background with insufficient fuel, the root issue is the same: a low energy availability state (LEA).
What We Used to Eat
Our grandparents didn't count macros—they just ate real food, and plenty of it. A typical day started with a huge farm breakfast: bacon, eggs, toast with butter and jam, fried potatoes, milk or juice, and often pancakes or oatmeal on the side. Then came a massive midday lunch with meat, mashed potatoes, buttered vegetables, and dessert—often pie or cake. Dinner wasn’t light either—think steak and potatoes, more bread and butter, a second slice of pie, and a glass of milk or sweet tea. People regularly drank carbohydrates in the form of milk, juice, lemonade, or sweet tea.
Compare that to today, where many people barely pick at a salad, sip coffee for breakfast, or fast until noon. We’ve normalized starvation while wondering why we’re anxious, constipated, freezing cold, infertile, or gaining weight on what used to be considered a starvation diet.
Here’s what’s even more shocking: this modern crisis of under-eating is brand new in human history. Our hunter-gatherer ancestors—including the Hadza tribe today—consumed roughly 2,500–3,000 calories per day for women, and 3,500–5,000 for men. Even just a few generations ago, in the 1940s and 50s, women averaged around 2,500 calories and men consumed between 4,000–8,000 depending on their jobs and manual labor. This wasn’t abnormal—it was necessary for survival, metabolic repair, reproduction, and resilience. And their bodies were leaner and more functional than ours.
What Went Wrong
Another massive factor? Fat. In the 1980s, Big Tobacco bought up most of the major food companies. Around the same time, the official definition of a "low-fat" diet quietly shifted—from 10% (as seen in primitive diets) to 30%. This change skewed decades of research. Our ancestors and traditional cultures like the Hadza often consumed as little as 10-15% of calories from fat, mostly from whole-food sources like lean meat, coconuts, and milk. Today, the average American diet is around 40% fat—and a shocking 20% of total calories now come from industrial seed oils, which were originally designed as machinery lubricants, not food.
Humans are not fat-burning animals. We are primates. And like most primates, we’re built to burn carbohydrates—especially fruit and roots—as our primary fuel source. We’ve done so for nearly 7 million years. Feeding our bodies a high-fat, low-carb, seed-oil-heavy diet is a radical, modern experiment. The result? A dramatic slowing of metabolism, widespread thyroid dysfunction, and rising rates of chronic illness.
So what changed? Seed oils entered the food supply. As we began storing more fat from damaged oils and losing our ability to metabolize properly, diet culture stepped in—telling us to restrict calories to lose weight. All it did was suppress our thyroid, lower our body temperature, and increase rates of chronic disease.
The average American body today doesn’t run at 98.6°F anymore. Most hover around 96.5–97.5°F. But here’s the kicker: every degree of temperature equals about 1,000 calories burned per day. So when our intake dropped from 2,500 to 1,500, our body dropped its temperature to match, assuming a famine had arrived. This is still the same hunter-gatherer body trying to survive. We became colder, sicker, and more metabolically fragile.
Even during the Minnesota Starvation Experiment in the 1940s—conducted at the University of Minnesota—women weighed an average of 120 pounds and ate over 2,500 calories. Men consumed 4,000–8,000 per day depending on their workload. Today, we call 1,800 calories “normal,” and people wonder why they feel terrible.
Before we go further, here’s a quick scan-and-go checklist to see if you might be one of the 90%:
Undereating Red Flags
You feel cold often (especially hands, feet, nose)
Waking temp <97.8°F, pulse <75 bpm
Bloating, constipation, or slow digestion
Dry skin, thinning hair, brittle nails
Irregular or missing periods
Sleep issues, especially early waking or light sleep
Anxiety, depression, or mood swings
Constant fatigue, no matter how much you sleep
Trouble building muscle or recovering from workouts
Low libido or hormonal symptoms
Frequent fungal, bacterial, or viral infections
Puffiness, sagging skin, or changes to facial shape
If even a few of these sound familiar, your metabolism may be downregulated—and reverse dieting could be the fix.
What most people don’t realize is that under-eating is one of the most pervasive and damaging health habits in modern society. It’s not just fatigue or a missing period—chronic low energy availability is behind the explosion in autoimmune diseases, insulin resistance, gut issues, infertility, insomnia, anxiety, and even facial changes like puffiness, skin sagging, and premature aging. When your body lacks fuel, it prioritizes survival over function: it shuts down digestion, slows thyroid output, impairs detoxification, and weakens immune defense. This creates the perfect storm for fungal and bacterial infections, food intolerances, hormonal imbalance, poor motility, and systemic inflammation. It also reduces stomach acid, bile flow, and enzyme output—leading to SIBO, fungal overgrowth, histamine reactions, and poor absorption of nutrients.
Long-term undereating is also one of the most overlooked root causes of mental health disorders. The brain, liver, and nervous system require high levels of glucose to function properly, and without it, mood, memory, and resilience all decline. This is why so many people report anxiety, depression, or burnout after months or years of keto or intermittent fasting. Low energy means low serotonin, low dopamine, low progesterone, low thyroid—and zero metabolic safety. If you’re not eating enough, your body knows it, and it responds accordingly: by breaking down.
What Is Energy Availability (EA)?
Energy Availability (EA) refers to the amount of energy left over for your body to run basic biological functions after exercise is accounted for. Your thyroid, fertility, digestion, brain, and immune system all depend on this leftover energy to function. When EA is too low, your body begins downregulating non-essential functions to conserve energy—leading to symptoms like cold intolerance, missed periods, fatigue, hair loss, and muscle loss.
For the numbers people: EA = (Total Calories – Exercise Calories) ÷ Lean Body Mass (kg)
<30 cal/kg EA = Low Energy Availability (LEA)
<20 cal/kg EA = Clinical starvation
~45 cal/kg EA = Minimum for hormonal/metabolic repair
50–55 cal/kg EA = Ideal for long-term health and performance
Translation: If you’re eating under 2,000 calories as a woman or 2,500–3,000 as a man, and you exercise at all, you might be operating with too little leftover energy—even if your weight is stable.
Who Needs Reverse Dieting?
Reverse dieting is the structured way to eat more without gaining excessive fat. It’s essential for anyone who’s been under-eating, whether intentionally or accidentally. If you’ve been dieting, fasting, or doing low-carb for too long, this is your path out.
You likely need a reverse if:
You’re under-eating (<2,000 for women, <2,500–3,000 for men)
You’re not building muscle or recovering from workouts
Your libido is low, your skin is dry, or your cycle is irregular
You feel cold, anxious, moody, or fatigued
You’ve followed keto, carnivore, fasting, or other restrictive protocols
If you like numbers: Under 45 cal/kg EA = metabolic stress, even if you're overweight. It’s not about your weight—it’s about how much energy your tissues get.
The 100-Calorie Rule: How to Reverse Safely
You can’t just jump from 1,500 to 2,500 overnight. Reverse dieting adds fuel slowly so your metabolism can speed up without triggering fat gain or digestive stress.
Start slow. Add 100 calories per week until you reach the minimum threshold of 43 cal/kg. After that, slow it down to 50-calorie increases until you reach 50–55 cal/kg for long-term health.
For example: 150 lbs, 30% body fat = 47.7 kg LBM
Minimum target: 47.7 x 43 = 2,051 kcal
Ideal target: 47.7 x 50 = 2,385 kcal
Simple version: If you’re a woman, aim to build up to 2,200–2,400+ kcal. Men: 2,800–3,200+. Take your time.
Macronutrient Priorities: Carbs and Protein First
When reverse dieting, what you eat matters just as much as how much. Most people need to drastically increase carbs and protein, while keeping fat low—especially if they’re coming from a high-fat, low-carb history.
Carbohydrates are essential for liver glycogen, thyroid conversion (T4 to T3), and leptin signaling. Protein supports tissue repair and lean mass preservation. Too much fat too soon can impair insulin sensitivity and stall metabolic recovery.
Macro guideline:
Carbs: 55–65% of intake
Protein: 2.0–2.2g/kg LBM
Fat: 10–15% of calories (30–40g/day)
Simple version: Eat more fruit, juice, tubers, dairy, and lean protein. Go easy on fats until you’ve restored metabolism.
Metabolism Metrics: Temperature and Pulse
You don’t need a lab test to track metabolic recovery. Two vital signs tell the story:
Waking body temperature: should be ≥97.8°F, ideally >98.0°F, and should reach around 98.6°F later in the day
Resting pulse: 75–85 bpm (higher is better here)
Low temps and low pulse = low T3 and slowed metabolism. These markers often improve before body composition does. They’re your green light that the plan is working.
Not a tracker? You should feel warmer, more relaxed, more energetic, and more resilient. That’s healing.
Athletes and Lifters: Muscle Doesn’t Grow in LEA
Trying to build muscle while under-eating is like trying to build a house without bricks. RED-S (Relative Energy Deficiency in Sport) is the name for what happens when athletes train hard but don’t eat enough. It’s not just a female athlete problem.
Symptoms include:
Plateaued lifts
Loss of motivation
Poor recovery and disrupted sleep
Injury or persistent soreness
To grow:
Maintain at least 45 cal/kg EA
Target 50–55 cal/kg EA for bulking phases
Simple version: Eat more than you think you need. Your performance will tell you when it’s working.
Eating Disorder Recovery: Refeeding = Restoration
In ED recovery, eating more isn’t just about weight gain. It’s about repairing the thyroid, restoring brain function, rebalancing hormones, and calming the nervous system. Recovery requires far more food than most people realize.
Most women need 2,500–3,000+ calories per day to fully heal. Using the EA model ensures you’re actually supporting your body instead of just gaining weight without true restoration.
Targets:
45–55 cal/kg EA
Minimum of 2,500 kcal/day for most
Simple version: You won’t fully heal unless you consistently eat enough. Full stop.
Timeline: How Long Does It Take?
There is no one-size-fits-all timeline. Some people reach the 43 cal/kg minimum in a month; others take longer depending on their digestive capacity, fear of weight gain, or metabolic symptoms. Refeeding tends to move quickly up to around 45–48 cal/kg, then slows down as the body adapts. It may take several months—or even a year—for someone to safely reach 50–55 cal/kg.
The goal isn’t to temporarily raise your intake, but to rebuild your baseline. This is your new maintenance, not something you "hold" and then drop. Once your body has recovered, you may strategically enter short cutting phases. But for most of your life, this is where your calories should live.
A general roadmap:
Begin by adding 100 kcal/week until you reach 43 cal/kg EA (which may take 4–8+ weeks)
After that, add 25–50 kcal/week until you approach 50–55 cal/kg EA (may take months)
Stay nourished consistently, without dropping below the 43–45 cal/kg threshold unless doing a short, strategic cut
You are only ready to attempt a fat loss phase when:
Temps are ≥98.0°F
Pulse is ≥75 bpm
Digestion, sleep, and mood are solid
No binge urges or extreme fatigue
Not a planner? Keep eating more until you feel alive again. That’s when healing locks in.
Summary: The Goldilocks Zone
If you’re cold, tired, wired, not sleeping, or not progressing in the gym, you’re likely in low energy availability. This applies no matter your weight.
Quick recap:
43–48 cal/kg = recovery zone
50–55 cal/kg = performance zone
<45 cal/kg = metabolic stress
10–15% fat = best starting point for most
Bottom line: If you want a thriving metabolism, you have to feed it. Consistently. Intentionally. Slowly.
Need help calculating your EA, macros, planning your reverse, or planning for a fat-loss phase? Work with a nutritionist who understands the science, the numbers, and the real-life struggles of eating enough to heal. I’ve lived it, tracked it, and coached dozens through it. Let’s build your body back—stronger than ever.
The Fungus Among Us
The Root Cause Doctors Rarely Acknowledge
Let me say this upfront: I had one of the worst systemic fungal and bacterial infections I’ve ever seen in a human body—and it was my own.
It started slowly. I had been keto for a couple years—thinking I was being “healthy.” But instead of feeling better, I started gaining weight. My digestion fell apart. I developed SIBO, constant bloating, and food intolerances. Looking back, I believe the low-carb, low-fiber, high-fat keto diet damaged my microbiome and starved my good gut flora, opening the door for overgrowth.
Then I "threw out my back." That’s what the ER told me, anyway. But the pain didn’t behave like a pulled muscle—it kept getting worse. Eventually, I discovered the truth: I had a bacterial infection in my spine, presenting as bulging discs and severe nerve pain. I was inflamed from head to toe.
From there, things spiraled.
I had chronic sinus and ear infections, alternating constipation and diarrhea, depression, anxiety, fatigue, and was down to only a handful of foods I could tolerate. But the worst of it came when I was breastfeeding. My daughter developed the worst thrush I’ve ever seen—her mouth looked like it was coated in cauliflower. My nipples were cracked, burning, and so painful I would scream into a pillow during feeds. But I refused to stop. I refused to give up. And I refused to switch to formula.
Instead, I spent months deep in research. Eventually, I cracked the code.
I figured out how to kill the fungus—without drugs. And once I healed myself, I knew I had to help others do the same.
Moldy Homes, Antibiotics, and Roundup: The Silent Triggers
Most people have no idea that mold exposure is almost guaranteed. Whether it’s a past leak, water damage behind the walls, or humidity buildup in the bathroom—mold spores and mycotoxins are everywhere, and once inhaled, they settle deep in your tissues.
Now stack that on top of multiple rounds of antibiotics—often prescribed for sinus infections, acne, or post-partum UTIs. These kill bacteria but leave fungus untouched, giving it free rein to overgrow.
And let’s not forget the glyphosate in our food supply—sprayed on non-organic wheat, oats, beans, and even many fruits and vegetables. Glyphosate wipes out beneficial gut bacteria and further weakens the terrain. Fungus loves the modern American body. We’re practically built to host it.
The Truth: Doctors Aren’t Trained for This
Here’s the hard truth: conventional medicine doesn’t recognize fungal overgrowth as a real diagnosis—let alone a systemic issue.
If you show up with fatigue, bloat, or brain fog, you might be offered an antidepressant. If you mention a recurring yeast infection, they’ll throw nystatin or Diflucan at it and call it a day. That’s the extent of their toolbox.
But those tools don’t work anymore. In the 70s, one Diflucan pill could knock out a yeast infection. I was once put on four a day for a month—and it did absolutely nothing. The fungus was resistant. And no one thought to ask why I wasn’t responding.
No one tested me for mold. No one mentioned the spine infection might be part of something bigger. No one ever considered that the entire terrain of my body was compromised—and fungus was running the show.
Why Herbs Work When Drugs Don’t
Once I realized the medical system had no answers, I turned to plants. And that’s when everything started to change.
Herbs work differently than pharmaceuticals. They’re complex, multi-layered, and synergistic. Fungus can’t mutate fast enough to outsmart an entire plant.
When I used herbs like grapefruit seed extract, berberine, garlic (allicin), oregano oil, caprylic acid, pau d’arco, and black walnut, I finally began to see results. The bloat started to recede. My energy returned. My daughter’s thrush began to clear. And for the first time in years, I felt like myself again.
Herbs didn’t just kill the fungus—they also helped with parasites, bacterial overgrowth, biofilm breakdown, and detox support. They worked with my body, not against it.
Die-Off Is Real (And You Shouldn’t Try This Alone)
Let me be honest: healing was not linear. When you start killing off fungal colonies, they release a storm of toxins—acetaldehyde, ammonia, mycotoxins—that overwhelm your liver, brain, and nervous system.
I went too fast in the beginning. I didn’t use binders. I didn’t support drainage. The die-off made me feel worse than before. That’s when I realized: this isn’t just about taking herbs—it’s about having a strategy.
Now, I guide others through this with support for detox pathways, liver drainage, lymphatic flow, and pacing—so the body can clear the debris without crashing.
Most Sinus Infections Aren’t Bacterial—They’re Fungal
Here’s a truth that could save you years of frustration: chronic sinus infections are almost always fungal in origin.
Doctors assume it’s bacterial, prescribe antibiotics, and send you on your way. But the relief is temporary—because they never address the fungal root. Fungus stays behind, forming colonies in the sinuses and middle ear, reactivating every time your immune system dips.
You’re not broken.
You’re just treating the wrong organism.
You Don’t Have to Do This Alone
I get it—I tried to DIY my healing, too. I read every blog, ordered every supplement, and still ended up flat on my back, bloated and brain-fogged, crying with pain during breastfeeding.
But once I had a real protocol—a functional, herbal, root-cause roadmap—everything changed.
And now I offer that roadmap to others.
Because you shouldn’t have to figure this out alone. Not when the system failed you. Not when you’re exhausted. Not when your body is screaming for help.
Ready to Heal the Root?
If you’re dealing with chronic sinus issues, bloating, anxiety, weight gain, food intolerance, or that mysterious feeling that something’s deeply off—you’re probably right.
And I want to help you fix it at the root.
Escaping the Swampland: How Low-Fat Diets Restore Metabolic Health
A very low-fat meal of chicken breast and roasted potatoes.
For years, the nutrition world has oscillated wildly between extremes—first vilifying fat, then idolizing it. Low-fat was once the gold standard, and then keto swooped in, promising effortless weight loss and boundless energy. But what if both sides missed something crucial?
As Denise Minger argued in her article In Defense of Low-Fat, we’ve thrown out a therapeutic tool that once delivered profound results. What if a very low-fat, high-carbohydrate diet (we're talking 10–15% of calories from fat) holds the key—not as a permanent way of eating, but as a metabolic reset? Evidence from forgotten clinical trials and powerful case studies shows that this approach can restore insulin sensitivity, reverse chronic illness, and reboot a damaged metabolism. Then, fat can be slowly reintroduced without regaining dysfunction.
Why Not Just Go Keto?
Low-carb and ketogenic diets can be effective at suppressing symptoms of metabolic dysfunction by removing carbohydrates, thereby reducing the need for insulin. But this doesn't mean the underlying issue—insulin resistance—is resolved.
In fact, long-term keto often leads to a condition known as physiological insulin resistance, where the body adapts to chronic carbohydrate deprivation by downregulating glucose uptake and storage. This is a protective, adaptive response—but it’s not without consequences. Over time, many keto followers develop signs of prediabetes, elevated fasting insulin, decreased thyroid function, and declining metabolic rate—even while continuing to restrict carbohydrates.
In other words, the damage can happen even if carbs are never reintroduced. Biomarkers may initially improve, but over time, thyroid function drops, stress hormones rise, and lipotoxicity—the accumulation of excess fat in organs and tissues—leads to chronic disease formation.
Then, when carbohydrates are reintroduced, things can get worse. Former keto dieters often experience blood sugar spikes, extreme fatigue, and rapid weight gain, even with modest carb intake. This isn’t just because they’re eating carbs again—it’s because their metabolism was never truly healed.
In contrast, low-fat, high-carb diets can retrain the body to use glucose effectively. They restore thyroid output, improve metabolic rate, and allow for metabolic flexibility.
WHY 10-15% FAT WORKS METABOLICALLY
What happens when you drop dietary fat to just 10-15% of your total calories? A lot more than you might think. This section summarizes five of the most well-established mechanisms explaining how very low-fat diets improve insulin sensitivity, metabolic rate, and overall health—even in the absence of calorie restriction or weight loss. Each mechanism is supported by peer-reviewed studies that collectively demonstrate how strategic fat reduction can rapidly restore glucose tolerance, repair thyroid function, and reduce the fat buildup in organs that drives chronic disease. These are not fringe ideas—they’re grounded in clinical evidence from both historic and modern trials.
To make this section easier to follow, each point includes a quick plain-language takeaway followed by a "Science Spotlight" for readers who want to dive deeper into the details.
1. Reduces Intramyocellular Lipids (IMCL)
Plain-language takeaway:
Cutting fat intake lowers fat droplets in muscle cells, improving insulin’s ability to help glucose enter cells.
Science Spotlight:
Total dietary fat—not just fat type—drives IMCL levels. In a 25‑day controlled feeding trial, subjects on a low-fat (≈31% energy from fat) diet had significantly lower muscle fat than on higher-fat diets (~36–38%). While the direct impact on insulin wasn't measured, this confirms that reducing dietary fat effectively lowers IMCL.
Study: St-Onge MP, et al. Am J Clin Nutr., 2007.
2. Lowers Lipotoxicity and Improves Mitochondrial Function
Plain-language takeaway:
Reducing dietary fat eases the fat burden on liver and pancreas, helping them function better—even before much weight is lost.
Science Spotlight:
In an 8‑week, 600 kcal/day liquid formula (20% fat) for people with type 2 diabetes, liver fat dropped ~70% and pancreatic fat declined significantly within a week. Insulin sensitivity and beta‑cell function were restored, supporting the “Twin Cycle” hypothesis
Study: Lim EL, et al. Diabetologia, 2011.
3. Improves Glucose Oxidation and Carb Tolerance
Plain-language takeaway:
When fat dominates, carb burning gets pushed aside. Lower fat intake lets the body efficiently use carbohydrates again.
Science Spotlight:
The Randle Cycle describes how high fat intake suppresses glucose oxidation. While we didn’t find a single big study to cite, decades of biochemical and clinical research confirm that lowering fat (and increasing carbs) shifts metabolism toward burning glucose more efficiently.
Foundational concept: Randle PJ, et al. Lancet, 1963. Also: Hue L, Taegtmeyer H. Am J Physiol, 2009.
4. Restores Thyroid Function + Reverses Adaptive Insulin Resistance
Plain-language takeaway:
High-carb, very-low-fat eating boosts active thyroid hormones (T3), improving metabolism and reversing the body’s adaptation to insulin resistance.
Science Spotlight:
Back in 1979, Danforth showed that switching to a high-carb, low-fat diet raised metabolic rate and increased thyroid hormone output—confirming early on that diet composition can “reactivate” thyroid function after low-carb suppression.
Study: Danforth E Jr., et al., 1979.
5. Reversal of Type 2 Diabetes Without Major Weight Loss
Plain-language takeaway:
You don’t have to lose huge amounts of weight to reverse diabetes. Cutting dietary fat—even while calories remain low—can restore blood sugar control in weeks.
Science Spotlight:
Lim’s 600 kcal/day formula diet—very low in fat—reversed diabetes in 11 obese patients: liver/pancreas fat fell ~30% in just 7 days, fasting glucose normalized, and beta-cell function was restored—all with only ~4% body weight loss
Study: Lim EL, et al. Diabetologia, 2011.
Low-Fat Isn’t What You Think It Is
Clinical low-fat diets that reversed disease used <10% fat, but modern “low fat” studies define it as 30% of calories—aka the swampland, a metabolic dead zone. This is Denise Minger's biggest point: we have redefined "low fat" in a way that neuters its therapeutic benefit.
She calls the middle zone a macronutrient swamp, where neither ketosis nor full-carb metabolism can happen cleanly. This is where modern Western diets live: moderate fat, moderate carb, high inflammation.
Why Fat Levels Should Shift With Your Metabolism
This approach uses phase-based fat manipulation, which mirrors what’s supported in the research. In the reset phase, fat is kept very low (~10%) to rapidly restore insulin sensitivity and reduce intramyocellular lipids and lipotoxicity. During the build phase, fat increases slightly (10–15%) to support glycogen storage and muscle growth while still maintaining insulin sensitivity. In the cut phase, fat stays low (10–12%) to accelerate fat loss without suppressing thyroid or metabolic rate. As you transition into the reverse phase, fat is slowly reintroduced (12–15%) while monitoring for signs of intolerance. Finally, in the maintenance phase, fat may rise to 15–30%, allowing for metabolic flexibility—if tolerated without compromising energy levels, digestion, or blood sugar.
How to Turn This Into a Metabolic Protocol
Here’s a strategic layout you can use for yourself or clients:
Metabolic Reset
Fat intake: 10% or less
Carbs: 70–75%, emphasis on fruit, juice, tubers, sugar
Protein: 15–20%, including collagen, dairy, lean meats
Goal: clear lipotoxicity, restore glucose oxidation, raise temps/pulse
Cut or Build (depending on body comp goals)
Fat: still 10–12% to maintain insulin sensitivity
Carbs: as high as tolerable
Protein: increased for muscle retention/building
Reverse and Maintenance
Slowly increase fat to 15–30% of calories
Monitor weight, body temp, libido, and mood
Add saturated fats first (dairy, cocoa butter), limit PUFA forever
Summary
Temporary fat reduction to 10% has been shown to reverse insulin resistance, MS, and heart disease
Fat impairs insulin signaling (via IMCLs), blocks glucose oxidation (Randle cycle), delays insulin clearance, and inflames organs like the pancreas and liver—even in healthy people
Restoring carb metabolism requires clearing IMCLs and lipotoxicity
“Low fat” = <10%, not 30% (which is the swamp zone)
Use this approach as a short-term metabolic reset, not a permanent solution
Slowly increase fat after the reset—up to 15–30% for long-term balance
The goal isn’t to stay low-fat forever. It’s to lose fat the right way—by restoring true metabolic health.
Let carbs and fat be friends again—but only after your body can handle it.
The Hidden Hypothyroid Cost of Low-Carb Diets
Low-carb diets promise a lot: quick weight loss, stable blood sugar, reduced cravings. And for a while, they deliver. But beneath the surface, a silent cost builds—especially for women. That cost is your thyroid.
Despite the early wins, long-term carbohydrate restriction can suppress thyroid function, reduce metabolic rate, and derail hormonal balance. The end result? A crash back to reality that often looks and feels like classic hypothyroidism.
Let’s break down what’s really happening—and how to spot it.
Why Carbs Matter for Thyroid Health
Carbohydrates play a direct role in the production and conversion of thyroid hormones:
Glucose is required for the conversion of T4 (inactive thyroid hormone) into T3 (the active, metabolism-boosting form).
Carbohydrate intake keeps liver glycogen stores full, which supports stable blood sugar and reduces cortisol output.
Without carbs, the body often elevates cortisol and adrenaline to maintain glucose levels—a state that suppresses T3 and slows metabolic function.
In short, your thyroid needs carbs to function properly. Depriving it long term is like trying to heat your house with the pilot light off.
Classic Symptoms of Low-Carb-Induced Hypothyroidism
Whether you’re keto, carnivore, or just living on meat and greens, here are the signs your metabolism may be tanking:
Cold hands and feet
Hair thinning or loss (especially in the shower or brush)
Constipation
Low body temperature (especially morning temps below 97.5°F)
Fatigue, even after a full night’s sleep
Brain fog or difficulty concentrating
Dry skin
Depression or emotional flatness
Low libido
Irregular or missing menstrual cycles
Weight gain despite low-calorie intake
These are not "normal aging." They're signs of a body running on survival mode.
Why Women Are Hit Harder
Women are particularly sensitive to drops in thyroid hormone and overall energy availability. Why?
Reproductive health depends on adequate thyroid and carbohydrate intake.
Female hormones (especially progesterone) require sufficient glucose to be produced and maintained.
The female body is wired to prioritize fertility and survival over fat loss—so when carbs drop, thyroid downshifts to conserve energy.
Many women on long-term low-carb diets experience amenorrhea (loss of periods), hypothyroid symptoms, and difficulty building or maintaining muscle mass. Some even lose their ability to tolerate carbohydrates at all—a condition known as physiological insulin resistance.
The Vicious Cycle of Carb Avoidance
Here’s the trap: low-carb lowers T3 and reduces your ability to metabolize carbs efficiently. Then, when you finally reintroduce carbs, your blood sugar spikes, you feel awful, and you assume carbs are the problem.
But they’re not. Your metabolism is just out of practice.
How to Heal: The Pro-Metabolic Alternative
The good news? You can rebuild. The key is to gently increase carbohydrate intake while supporting thyroid function and reducing stress.
Start with:
Whole fruit, root vegetables, and honey
Bone broth and gelatin for glycine and gut support
Dairy (if tolerated) for calcium and fat-soluble vitamins
Salt for adrenal support
Nutrients like magnesium, selenium, and vitamin A
Aim for consistent, balanced meals with protein, carbs, and a little fat. And track your body temperature—it’s a real-time window into thyroid health.
Bottom Line
Low-carb diets may feel like magic in the beginning, but long-term they can cost you your thyroid, your cycle, and your spark.
If you’re cold, tired, and stuck—don’t double down on restriction. Rebuild with carbs. Reignite your thyroid. And reclaim the energy your body was meant to have.
Scientific References
1. Carbs and T3 Conversion
Study: Effects of caloric and carbohydrate restriction on thyroid hormone metabolism in obese patients.
Source: The Journal of Clinical Endocrinology & Metabolism, 1982.
Link: https://doi.org/10.1210/jcem-54-2-386
Summary: Carbohydrate restriction significantly reduced serum T3, even when total calories were adequate. Low-carb diets suppressed active thyroid hormone conversion.
2. Low-Carb Increases Cortisol and Stress Hormones
Study: Cortisol is elevated during ketosis in lean and obese humans.
Source: The Journal of Clinical Endocrinology & Metabolism, 1994.
Link: https://doi.org/10.1210/jcem.79.6.7989461
Summary: Low-carb diets increase cortisol levels, likely to maintain blood glucose through gluconeogenesis in the absence of dietary carbs.
3. Physiological Insulin Resistance on Low-Carb
Study: Insulin resistance is a physiological response to reduced carbohydrate availability during ketogenic diets.
Source: Nutrition & Metabolism, 2009.
Link: https://doi.org/10.1186/1743-7075-6-2
Summary: Long-term low-carb diets can cause physiological insulin resistance, making it harder to tolerate carbs upon reintroduction.
4. Women’s Hormones, Fertility, and Carb Availability
Study: Effects of carbohydrate restriction on reproductive hormones in healthy women.
Source: American Journal of Clinical Nutrition, 2007.
Link: https://doi.org/10.1093/ajcn/85.3.779
Summary: Reduced carbohydrate intake lowered LH, estradiol, and progesterone levels, disrupting ovulatory function.
5. Thyroid and Energy Availability
Study: Low energy availability suppresses thyroid function and menstrual cycle in women.
Source: Medicine and Science in Sports and Exercise, 2000.
Link: https://doi.org/10.1097/00005768-200005000-00015
Summary: Women with chronically low energy availability had reduced T3 levels and disrupted reproductive hormones.
6. Glycogen and T3 Regulation
Study: Hepatic carbohydrate metabolism and the control of thyroid hormone metabolism.
Source: Trends in Endocrinology and Metabolism, 2000.
Summary: Liver glycogen stores are necessary for efficient T4 to T3 conversion; depleted glycogen impairs this process.