Cold Plunges, Cortisol, and Carnivore: The Biohacked Burnout of Carb Deficiency
You don’t have adrenal fatigue. You have a glucose deficiency.
I just listened to the Joe Rogan x Gary Brecka interview from a few months ago, and by the end of it, I felt like I was eavesdropping on two men trying to survive a famine — one cold plunge and ozone sauna at a time.
No one said the word “cortisol” once. Not in a 2.5-hour conversation about stress, optimization, morning routines, energy crashes, and biohacking.
Not. One. Time.
But that’s exactly what this was: a full-length, high-production podcast episode on how to manually override your biology when your body is running on stress hormones 24/7 because you refuse to eat a carbohydrate.
The Carnivore Grind: Steak for Breakfast, Stress for Dessert
You know the type.
Shawn Baker, Anthony Chaffee, Ken Berry — the poster boys of "peak performance" on a diet of nothing but ribeyes, butter, and beef liver.
No carbs. No sugar. No fruit.
But plenty of cortisol.
Let me say it plainly: these men are not thriving.
They are surviving — on adrenaline, norepinephrine, and every biohack under the sun.
You see them chugging coffee, skipping meals, hitting the cold plunge at 5am, blasting red light at their faces, popping testosterone injections, taking metformin “for longevity,” meditating while wired and inflamed, bragging about how they haven’t had a carb since 2003...
That’s not health. That’s crisis management.
Cold Plunges Are a Symptom, Not a Solution
Don’t get me wrong — I love a good cold plunge. But let’s be honest about what it is:
It’s a sympathetic nervous system bomb.
If you need a freezing tub of water, followed by coffee, followed by red light therapy, just to feel alive — you're not optimizing. You're desperately chasing the dopamine your nervous system is too depleted to produce.
And if you’ve been living in ketosis long enough, that might be the only way to feel anything at all.
Cortisol Is Carrying You (and You’re Calling It Discipline)
Carbohydrate deficiency triggers a predictable cascade:
Liver glycogen tanks.
Blood sugar drops.
The body panics.
Adrenal glands crank out cortisol to keep you conscious.
At first, you feel “clear-headed,” “sharp,” maybe even “unstoppable.”
Because cortisol feels good — for a while.
Until it doesn’t.
Eventually you crash:
Insomnia
Constipation
Blood sugar swings
Anxiety
Tanked testosterone
Fatigue so deep it takes an ozone chamber and 16 supplements just to take a poop
This isn’t vitality. It’s just living off your stress hormones.
The Truth About Carnivore "Optimization"
Let’s talk about the carnivore influencers.
A recent comment from Jay Feldman or Mike Fave (I forget which, they both crush) mentioned that Shawn Baker’s testosterone is allegedly bottomed out. Like… dangerously low.
How does that happen to a guy who lifts every day and eats nothing but steak?
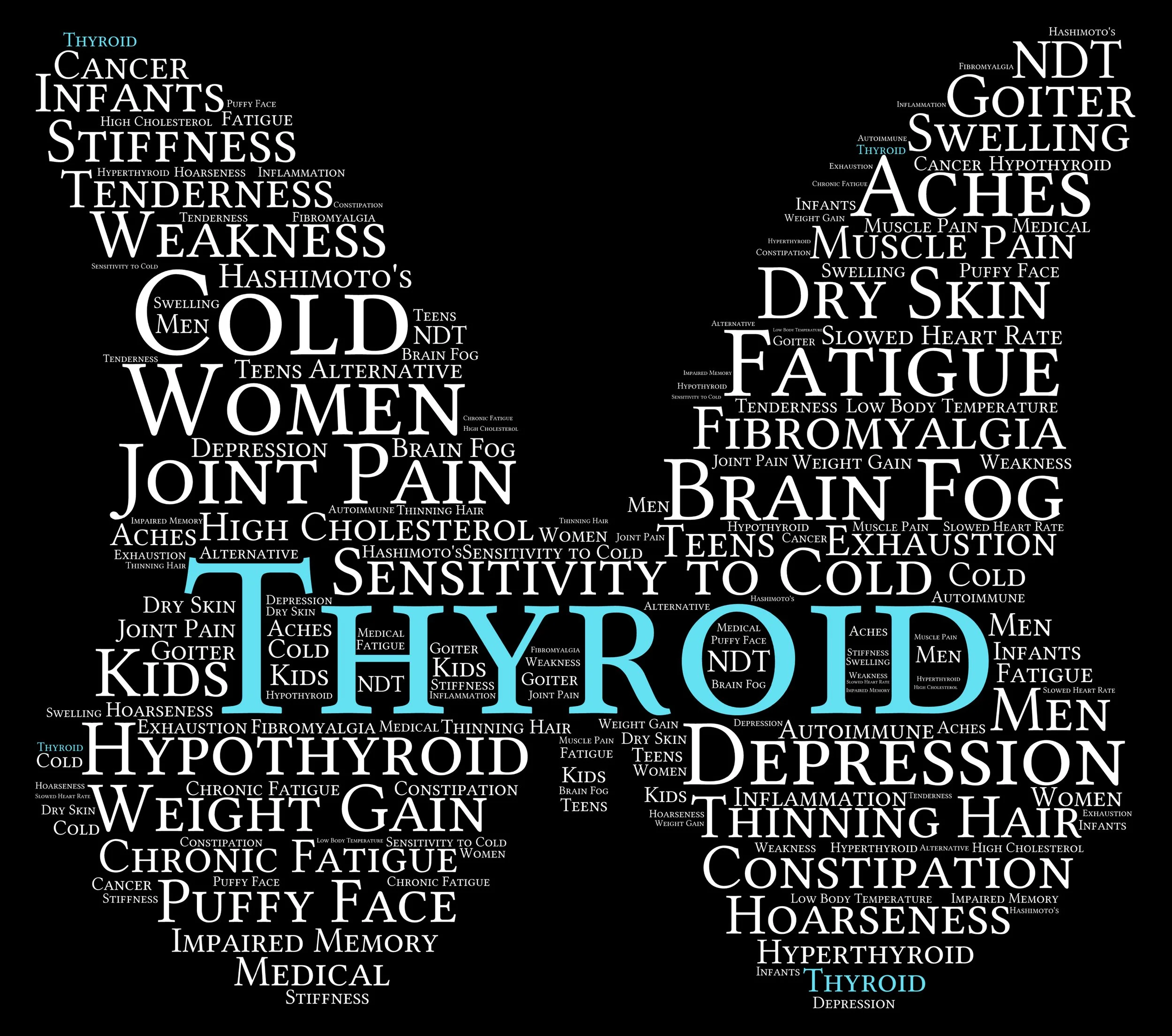
Simple: no carbs = no insulin = no conversion of thyroid hormone = no signal to the testes = no testosterone.
Yes, you can look shredded while running on fumes.
Yes, you can build muscle while slowly tanking your metabolism, hormone function, and mental health.
But you won’t feel good. And it won’t last.
I Was There Too
I’m not writing this from the outside. I lived it.
I was keto for eight years — hardcore. The last year of that, I went full carnivore. I hadn’t eaten more than 20 grams of carbs a day in nearly a decade. I lived off ribeyes and coffee, and listened religiously to every podcast Paul Saladino put out.
And then, one day, I heard him talking about the dangers of long-term carb restriction — and it hit me like a truck. Every symptom he described? I had it:
Muscle cramping
Morning anxiety
Insomnia
Low libido
Cold hands and feet
PMS from hell
Joint pain
Depression
Constipation
Eventually I tested my thyroid and found out my T3 was low — the missing puzzle piece that made everything make sense. I was stuck in survival mode, living off cortisol, pretending it was “discipline.”
So I did something radical:
I added back carbohydrates. Not all at once, but in small, steady amounts, spaced throughout the day. Within weeks, every single symptom started to disappear. My mood stabilized. I could sleep. My cycle regulated. My body warmed up. I came back to life.
Carbs Are Not the Enemy — They’re the Missing Piece
Carbs are not toxic.
Sugar does not “feed disease.”
Fruit is not why you’re tired.
You’re tired because your mitochondria haven’t seen glucose since Obama was in office.
Carbohydrates are:
The body’s preferred fuel
The thyroid’s best friend
The antidote to cortisol
The fuel for progesterone, serotonin, dopamine, and testosterone
You don’t need another cold plunge.
You need orange juice.
Summary — The Biohacked Burnout Checklist
Cold plunges are a cortisol crutch
Carnivore = constant stress signal
Low-carb = low testosterone, low thyroid, low mood
Biohacking is just symptom suppression in disguise
Real energy starts with eating carbs — not avoiding them
Final Thought
If you need an elaborate “morning routine” to feel functional… you’re probably missing the most basic routine of all:
Eat carbs. Often. Especially in the morning.
You don’t need 10 supplements, 3 gadgets, and a neurofeedback helmet.
You need glucose.
Sip Your Way to Stable Blood Sugar
Why Drinking Protein + Carb Mini Meals Works
Small sips, big impact. Support your thyroid, lower stress hormones, and hit your macros without bloating.
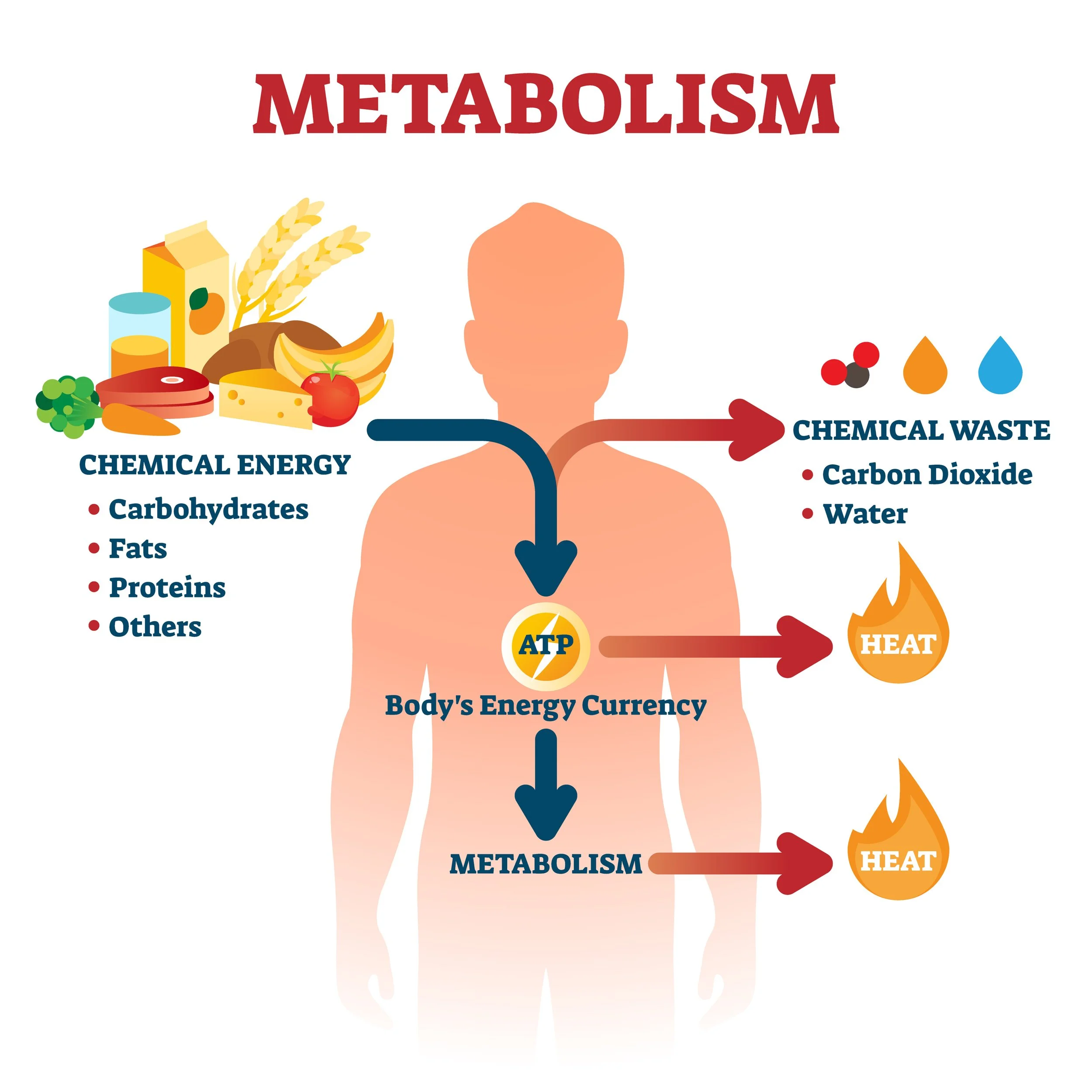
For years, mainstream nutrition pushed three square meals a day—or worse, fasting windows and long gaps between meals—as the gold standard for “metabolic health.” But if you’re healing your metabolism, restoring energy availability, or trying to lose fat without tanking your thyroid, there’s a better way. And it might be hiding in your blender.
Enter: liquid protein + carb mini meals, spaced throughout the day.
We’re talking 6 small meals every 2–3 hours, mostly drank—not chewed. Think orange juice and collagen, skim milk and honey, smoothies with fruit and nonfat Greek yogurt. These aren’t meal replacements. They’re strategic tools to keep your metabolism humming, blood sugar stable, and stress hormones low—especially during a cut or a healing phase.
Why It Works: Blood Sugar, Cortisol, and Energy Efficiency
Eating small, frequent meals that combine protein + carbs:
Prevents blood sugar crashes
Stable glucose = stable mood, fewer cravings, and better willpower.
Blunts cortisol spikes
Every time you go too long without food, cortisol kicks in to raise blood sugar via gluconeogenesis. That’s muscle-wasting, thyroid-suppressing, and metabolism-slowing. No thanks.
Supports the thyroid
Your thyroid needs sugar and aminos throughout the day to produce T3 and keep your temps up.
Boosts digestion
Liquid meals are gentler on the gut. For anyone healing from SIBO, IMO, or low stomach acid, they’re easier to digest and absorb—especially when fiber is temporarily reduced.
Spreads out your macros
You can hit your targets (especially high carb + low fat) without bloating or overwhelming your system in one sitting.
Metabolic Benefits on Tap
This isn’t about grazing or snacking. These sippers are metabolically strategic mini meals designed to:
Protect lean muscle
Stabilize blood sugar
Keep your liver and thyroid fueled
Maintain mood, energy, and focus
Hit macro targets (especially during a cut or reverse diet)
Who Benefits Most?
Anyone in a cut
Fewer calories = less room to feel full. Drinking your meals makes it easier to avoid hunger while still packing in nutrients.
People recovering from LEA (low energy availability)
Small meals reduce the burden on digestion and keep fuel flowing to the cells.
Anyone with poor appetite or hypoglycemia
Liquid meals go down easier and stop the blood sugar rollercoaster.
Athletes and busy professionals
No cooking, no cleanup. Shake it and sip.
What to Drink: Meal Ideas
High-carb, low-fat, bloat-free & metabolism-friendly
Use these between whole-food meals to hit your macros, or build your entire day around them if you're in a deep cut or digestive flare.
Orange Julius Smoothie
6 oz orange juice
1/2 cup nonfat Greek yogurt
2 tbsp collagen
Splash vanilla extract
~22g protein, 32g carbs, 0g fat
Maple Milk
1 cup skim milk
2 tbsp collagen
1 tbsp maple syrup
Dash vanilla + pinch salt
~22g protein, 25g carbs, 0g fat
Maple Collagen Latte
1 cup strong brewed coffee or 2 shots espresso
1 cup skim milk
1 tbsp maple syrup
2 tbsp collagen
~22g protein, 25g carbs, 0g fat
Blend or froth for that creamy café vibe—perfect pre-walk or AM blood sugar support.
Metabolic Chocolate Milk
1 cup skim milk
2 tbsp collagen
1 tsp unsweetened cocoa
1 tsp honey
~20g protein, 20g carbs, 1g fat
Strawberry Yogurt Shake
1/2 cup nonfat Greek yogurt
1/4 cup strawberry lemonade
2 tbsp collagen
Splash water or coconut water to thin
~25g protein, 20g carbs, 0g fat
Tropical Glow Smoothie
1/2 cup pineapple juice
1/2 cup frozen mango
1/2 cup nonfat Greek yogurt
2 tbsp collagen
Squeeze of lime + pinch salt
~22g protein, 32g carbs, 0g fat
Peaches & Cream Sipper
1/2 cup canned or stewed peaches (in juice, drained)
1/2 cup lowfat cottage cheese or nonfat Greek yogurt
1 tbsp maple syrup or honey
Dash cinnamon (optional)
Splash of water or almond milk to thin
~22g protein, 28g carbs, 1–2g fat
Carrot Cake Elixir
1/2 cup carrot juice
1/2 cup skim milk
2 tbsp collagen
1 tbsp maple syrup
Dash cinnamon + pinch salt
~22g protein, 28g carbs, 0g fat
Fat Loss Without the Stress
When you're in a fat loss phase (or just trying to maintain muscle while trimming down), the biggest enemy isn’t calories—it’s stress. Frequent protein + carb meals are your anti-stress armor. They prevent the body from shifting into catabolic mode, where it burns muscle, lowers thyroid, and stores fat out of survival.
A stable metabolism is a flexible one—one that trusts it will be fed consistently and doesn’t panic. That’s how you lose fat without the insomnia, hair loss, fatigue, or rebound.
Why Sip Mini Meals?
✔ Easier to digest
✔ Blunts hunger and cortisol
✔ Keeps blood sugar stable
✔ Helps hit high-carb/low-fat targets
✔ Protects thyroid, muscle, and mood
✔ Keeps energy steady during healing or a cut
Whether you’re deep in a cut or climbing out of burnout, sipping your meals might be the metabolic magic trick you were missing.
🍫💪 Chocolate Collagen Milkshake Magic: 4 Dreamy, Metabolism-Supporting Flavors
🔥 Blood sugar–steadying, metabolism-loving, and ridiculously good.
Rich, creamy, low-fat, and packed with protein + carbs—these collagen milkshake-style blends are designed to support your thyroid, stabilize blood sugar, and give you a satisfying treat without crashing your energy or hormones.
Each one starts with a pro-metabolic base:
🥛 Skim or low-fat milk for calcium, carbs, and sleep support
💪 Collagen for gut lining, joints, skin, and hair
🧁 Maple syrup or honey for glucose and glycogen replenishment
🍫 Optional cocoa or coffee for flavor and fuel
🧂 Salt + 🌿 vanilla to bring it all together
✨ Base Recipe:
🍫🥜 Cocoa Peanut Butter Cup Collagen Milk
A nostalgic milkshake flavor—with metabolic benefits.
Sweet, creamy, and decadent without the junk or seed oils. Peanut powder adds protein and flavor with virtually no fat, making this a perfect mini-meal.
Ingredients:
1 cup skim raw milk (or low-fat raw milk or milk of choice)
2 tbsp collagen
1 tbsp peanut powder (Organic PB2 or equivalent)
1 tsp cocoa powder
1 tbsp maple syrup
1/4 tsp vanilla extract
Dash of sea salt
Directions: Blend until smooth. Serve over ice or gently warmed. Enjoy mid-morning or afternoon.
☕ Variation #1: Mocha Peanut Butter Cup
Chocolate + coffee + peanut butter? Yes, please.
Add 1/2 - 1 cup strong brewed coffee or 1–2 shots of espresso
Keep all other ingredients the same
This variation makes a fantastic pre-workout or productivity booster.
☕️🍫 Variation #2: Classic Mocha Collagen Milk
No peanut, just chocolate and coffee.
Omit the peanut powder
Add 1/4–1/2 cup brewed coffee or espresso
Keep the cocoa, collagen, and sweetener
Think clean Starbucks mocha without the dairy, PUFA, or sugar crash.
🍌 Variation #3: Chunky Monkey
Chocolate + banana = creamy, dreamy, potassium-packed.
Omit peanut powder
Add 1/2 of a ripe banana (fresh or frozen)
Keep cocoa, collagen, and maple syrup
Optional: Add cinnamon or a dash of nutmeg for extra warmth.
🍯 Variation #4: Salted Caramel Collagen Milk
Buttery-sweet flavor with none of the junk.
This one hits all the comfort buttons—sweet, salty, cozy—with a dreamy caramel vibe that feels like dessert. Bonus: it’s still low-fat, PUFA-free, and packed with collagen + calcium.
Omit:
Peanut powder
Cocoa powder
Add:
1–2 drops caramel extract OR swap the maple syrup for 1 tablespoon of real caramel sauce made with cane sugar and no seed oils, I like this one.
Keep or slightly increase the sea salt to enhance the caramel flavor
Optional: a pinch of cinnamon for warmth
Optional: Add a pinch of cinnamon for a warm, toasted note.
💖 Bonus Flavor Ideas:
Perfect for seasonal swaps or rotating new options into your mini-meal lineup:
🍓 Strawberry Cream: 1/2 cup strawberries + honey + vanilla
🍥 Coconut Caramel: Add a dash of coconut extract + maple
🎂 Birthday Cake: Use butter + almond extract + vanilla
🍎 Apple Pie: Add applesauce + cinnamon + honey
🍑 Peaches & Cream: Use ripe peach + vanilla + maple syrup
🥤Metabolic Milkshakes: Sipable Mini Meals for Energy + Hormones
Metabolic Mini Meal Sipper (Master Recipe + Flavor Variations)
A low-fat, high-carb protein + carb drink to support blood sugar, thyroid, and muscle during fat loss or healing. Blend or shake and sip every 2–3 hours.
🔧Master Formula
1 cup liquid (skim milk, fruit juice, carrot juice, or lemonade)
2 tbsp collagen or gelatin
1/2 cup protein source (nonfat Greek yogurt or lowfat cottage cheese)
1 tbsp natural sweetener (maple syrup, honey, or stewed fruit)
Flavor add-ons (spices, cocoa, fruit, citrus, vanilla, pinch of salt)
🧬 Macros: ~20–25g protein, 20–35g carbs, 0–2g fat
🍊 Orange Julius
6 oz orange juice
1/2 cup nonfat Greek yogurt
2 tbsp collagen
Splash vanilla + pinch of salt
🍁 Maple Milk
1 cup skim milk
2 tbsp collagen
1 tbsp maple syrup
Dash of vanilla + pinch of salt
☕ Mocha Latte
1 cup strong coffee or 2 shots espresso
1 cup skim milk
2 tbsp collagen
1 tsp cocoa powder + 1 tbsp maple syrup
🍫 Chocolate Peanut Butter
1 cup skim milk
2 tbsp collagen
1 tsp cocoa powder
1 tbsp peanut powder
1 tsp honey
🐒 Banana Cream
1/2 banana
1/2 cup nonfat Greek yogurt
1/2 cup skim milk
2 tbsp collagen
Dash cinnamon + pinch salt
🍑 Peaches & Cream
1/2 cup canned peaches (in juice, drained)
1/2 cup lowfat cottage cheese
1 tbsp maple syrup
Splash almond milk to thin + dash cinnamon
🍓 Strawberry Yogurt
1/2 cup nonfat Greek yogurt
1/4 cup strawberry lemonade
2 tbsp collagen
Splash coconut water to thin
🥕 Carrot Cake
1/2 cup carrot juice
1/2 cup skim milk
2 tbsp collagen
1 tbsp maple syrup
Dash cinnamon + pinch salt
🌴 Tropical Glow
1/2 cup pineapple juice
1/2 cup frozen mango
1/2 cup nonfat Greek yogurt
2 tbsp collagen
Squeeze lime + pinch salt
Whether you’re deep in a cut or just trying to keep your energy stable while healing, sipping your meals might just be the metabolic magic trick you were missing.
Why Gut Issues Often Return During a Cut
If you’re finishing a fat loss phase and suddenly feel like your digestion is worse—bloating, gas, constipation, food sensitivities flaring up—you’re not crazy. But let’s be very clear: this is not a sign that carbs are the problem. It’s a sign that your gut—and your entire body—is still in a malnourished state.
I see this all the time with clients. They’ve been cutting for 4–6 weeks, running on lowered energy availability, and the minute we start refeeding or adding carbohydrates back in, gut issues resurface. Their first instinct? “The carbs are causing it.” I hear the panic:
“It must be the sourdough.”
“I’m feeding candida again.”
“I think I need to go back to keto.”
No. Let’s break this down.
Cutting Starves the Gut—Literally
A cut isn’t just a reduction in energy. It’s a drop in micronutrients, fiber, fermentable substrates, and metabolic signals like T3. It’s a famine state. And guess who else goes hungry?
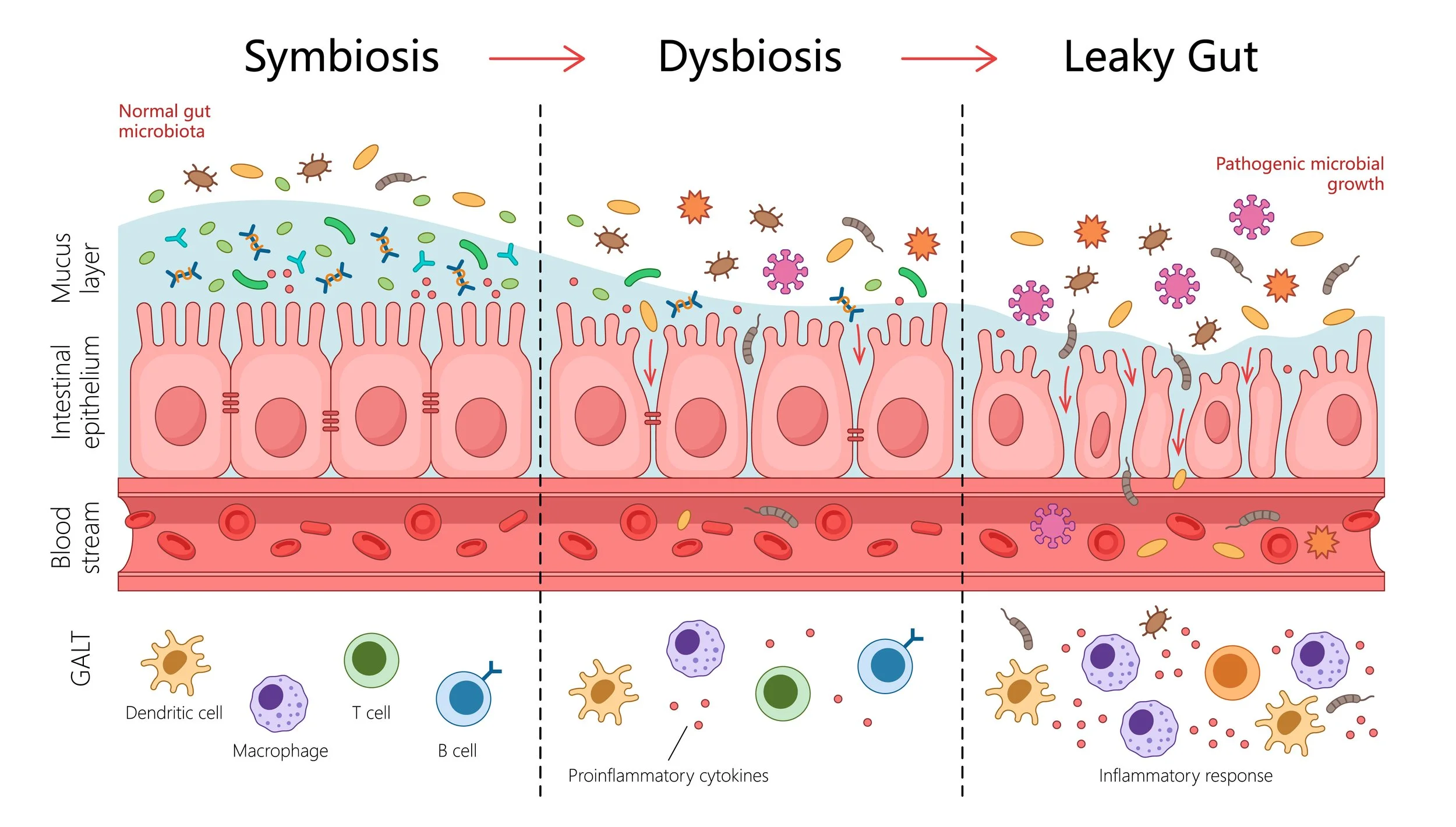
Your gut bacteria.
During a cut, your beneficial microbes—the ones that keep pathogens in check and maintain the gut lining—get underfed. And when that happens, two things start to unravel:
The mucosal barrier thins.
The immune system downregulates.
Digestion slows down—because the body shunts energy toward more essential systems like the brain, heart, and muscles, leaving less fuel for enzyme production, bile flow, and peristalsis.
This creates an opening for pathogenic or opportunistic microbes to sneak in or re-establish dominance. So when you reintroduce carbs—especially fermentable ones—you might feel worse not because you’re feeding the “bad bugs,” but because you’re finally feeding the good ones, and they’re trying to reclaim territory.
That process? It’s called die-off. Or more accurately: a Herxheimer reaction.
Die-Off ≠ Overgrowth
Die-off symptoms—fatigue, mood swings, bloating, skin flares, weird body odor, changes in bowel movements—often mimic what people assume are “overgrowth” symptoms. But this isn’t a sign of fungal relapse or bacterial disaster. It’s a war. And the good guys are winning.
When you increase carbohydrates, especially after a long period of underfeeding, you:
Reawaken dormant digestive fire (T3 rises)
Stimulate bile and enzyme production
Feed SCFA-producing bacteria (SCFA = short-chain fatty acids, like butyrate and acetate, which strengthen the gut lining, reduce inflammation, and improve motility)
Starve out methane-producing archaea and sulfate-reducing bacteria by increasing gut movement
Yes, this process is uncomfortable. But it is necessary for long-term gut repair.
Not All Carbs Are Created Equal (Especially After a Cut)
A huge mistake I see? Clients try to reintroduce the same types of carbs they thrived on at maintenance—sourdough, white rice, salads, berries with seeds, potato skins, cassava, even sprouted oats or whole fruits with lots of fiber. But post-cut digestion is fragile. T3 is still suppressed, enzyme output is low, and motility is sluggish.
What digests well at maintenance might wreck you during refeed.
This is not a sign that you’re broken. It’s a sign to shift strategy.
The Best Carbs for Gut Repair (Refeed Edition)
Your digestion during a refeed is not “normal.” It is compromised, sluggish, and healing. Here’s how to approach carbs during this fragile but critical rebuilding window:
Stick to the easiest-to-digest carbs:
Liquid carbs: fruit juice, coconut water, organic lemonade, Italian soda (cane sugar), kombucha (if tolerated), honey, maple syrup, and skim milk (raw is best)
Whole fruits that have low fiber and seeds: mango, melons, stone fruit like peach and plum
Cooked, peeled tubers like sweet potato or white potato (only if well tolerated)
Fiber carbs must be well tolerated. Avoid if they cause symptoms:
Sourdough (even well-fermented)
White rice (especially for those with methane archaea or IMO)
Berries with seeds
Potato skins
Sprouted oats
Raw salads
Cassava
Any raw or undercooked fibrous vegetables
Your gut may handle these better after 2–4 weeks of consistent refeeding with easier carbs.
Important: Everyone digests carbs differently.
Your ability to digest carbohydrates depends on your bacterial diversity, enzyme output, and even stress levels. What works for one person (white rice, sourdough, beans) may not work for another. I always recommend starting with the simplest carbs and slowly layering in fiber once symptoms stabilize and metabolic markers (like body temp and motility) improve.
The Mental Trap: Blaming Carbs
Most of us have internalized decades of carb-phobia. So when digestion goes haywire, it’s easy to fall back on the belief that carbs are to blame. But let me say this bluntly:
It’s not the carbs. It’s the malnourishment.
Carbs didn’t cause your weight gain. Swampland did (that high-fat/high-carb no man’s land where nothing burns efficiently).
Carbs aren’t triggering your yeast. They’re triggering your immune system to respond as your gut terrain shifts.
If anything, the cut—especially one done with moderate to high fat—is what destabilized your microbiome in the first place.
The Refeed Feels Worse Than the Cut (And That’s Normal)
Most people expect to feel better when refeeding. More food = better, right?
Not always.
Early refeed can be even harder than the cut itself, because your body is still downregulated:
Metabolism is low (T3 takes time to rebound)
Digestion is weak (enzymes are sluggish)
Detox pathways are backed up (no bile, poor methylation)
Gut bugs are fighting for dominance
You’re still technically in a malnourished state. But now you’re introducing fermentable fuel. This combo can trigger temporary chaos.
The key? Push through—gently. Don’t overdo fiber. Don’t crank fat back up. Stick to simple carbs and digestible foods. Trust the process. You’re rebuilding.
My Pro-Metabolic Refeed Rules for Gut Repair:
Keep fat ultra-low during early refeed (0.3–0.4 g/kg)
Use simple, low-residue carbs (fruit juice, maple syrup, coconut water, Italian soda)
Split carbs across 4–5 meals/day for blood sugar and motility
Support detox with daily raw carrot or bamboo shoots
Temporarily avoid high-fiber carbs unless well tolerated (sourdough, berries with seeds, sprouted grains, etc.)
Gradually layer in cooked, peeled tubers only if tolerated
Track symptoms and metabolic markers (temps, pulses, stools)
Don’t fear a little bloat or gas—it’s part of the rebuild
Summary:
Gut issues after a cut aren’t because of carbs—they’re because of the cut.
Carbs feed beneficial bacteria that repair the gut lining and outcompete pathogens.
The refeed can trigger die-off, not overgrowth—don’t confuse the two.
Your digestion is compromised post-cut, even for foods you normally tolerate.
Stay low-fat, stick to easy carbs, and allow time to heal.
And most importantly: your gut needs nourishment, not another restriction cycle.
Jaggery: The Forgotten Sweetener That Actually Nourishes You
When most people talk about sugar, it's either demonized as the root of all evil or worshipped in its raw, crunchy, coconut form. But somewhere between the extremes of white sugar and bitter blackstrap molasses, there’s a forgotten hero of mineral-rich sweetness: jaggery.
Never heard of it? You’re not alone. But if you’ve been chasing the pro-metabolic life and want a sweetener that actually does something for your body, jaggery deserves a place in your pantry.
So… What Is Jaggery?
Jaggery is an unrefined sugar made by boiling down sugarcane juice (or occasionally date palm sap) into a thick, sticky, mineral-rich paste that’s dried and molded into blocks or powder. The key difference?
The molasses stays.
That means jaggery contains both the sugar and the minerals in one whole-food package.
Unlike white sugar, which is stripped, bleached, and purified into pure sucrose — and unlike brown sugar, which is basically white sugar with a little molasses added back in as an afterthought — jaggery is the real deal. It’s how sugar used to be.
Nutritional Breakdown
Per tablespoon, jaggery offers a surprising dose of:
Iron (especially useful if you're healing from anemia or menstruating)
Calcium + Magnesium (mineral support for bones, thyroid, and adrenals)
Potassium (key for hydration, insulin sensitivity, and blood sugar stability)
B Vitamins (small amounts of B6, B2, B1)
Still a sugar? Yes. But it’s a sugar your body recognizes — not just a calorie bomb with nothing to offer.
Pro-Metabolic Uses
Jaggery isn’t just a sweetener — it’s a functional food. I recommend it to clients who:
Are healing from low iron or adrenal fatigue
Want a whole-food source of sweetness with actual value
Need a pre-workout glucose bump without the crash
Are transitioning off refined sugars or artificial sweeteners
Want to improve insulin sensitivity without overloading on pure sucrose
Favorite ways to use it:
Stir into tea or coffee (just like honey)
Add to warm milk with collagen for a mineral-rich bedtime treat
Use in energy balls with gelatin and coconut flour
Melt into oatmeal or mashed sweet potatoes
Mix with ghee for a traditional Ayurvedic immune booster
What to Watch For
Some jaggery on the market is adulterated with white sugar or made in unsanitary conditions. Look for:
Certified organic or traditional handmade jaggery
Ingredients: 100% cane juice or date palm sap
Block, paste, or powder form with no additives
Summary
Jaggery = whole cane sugar + molasses + minerals. Unlike white sugar, it feeds your cells — not just your cravings. It’s rich in iron, potassium, magnesium, and B vitamins. Use it in moderation like you would honey or maple syrup, but know you’re actually supporting metabolism with every bite.
Real Sweeteners Do Real Things
In the pro-metabolic world, we don’t fear sugar — we respect it. The type of sugar matters. If you’re still spooning white sugar into your coffee or pretending brown sugar is “less bad,” it might be time to meet jaggery.
She’s ancient, mineral-rich, and here to nourish your cells — not rob them.
What Did Hunter-Gatherers Really Eat?
Spoiler: It Wasn’t Grains, Almonds, or Bacon
For decades, the public has been sold a fantasy version of the “paleo diet.” Flip through a popular paleo cookbook and you’ll see heaping plates of ribeyes, piles of nuts, and endless “grain-free” breads made with almond flour. This glossy picture has almost nothing to do with what our ancestors actually ate. If you want the truth about human metabolism and ancestral nutrition, you have to step away from modern reconstructions and look at the real evidence from living hunter-gatherers, primate biology, and archaeology. The reality is both surprising and liberating: our ancestors weren’t keto, and they weren’t scarfing down handfuls of almonds. They were carb-powered primates who lived on honey, fruit, roots, and modest amounts of animal food—with very little fat.
Grains and Nuts: Modern Myths About Ancient Foods
Let’s start with what they didn’t eat. The idea that hunter-gatherers survived on wild grains is mostly projection. Wild grains existed, but they were small, bitter, and packed with antinutrients. They required extensive processing—pounding, grinding, soaking—to yield meaningful calories. Grinding stones have been found in the archaeological record, but this proves only that early humans could process grains, not that they were staples. At best, grains were fallback foods in times of scarcity, not everyday fare. Agriculture only made grains truly accessible by breeding them into larger, sweeter, less toxic varieties.
Nuts are another modern misconception. Today’s almonds, walnuts, and cashews are heavily domesticated, bred to be palatable and high-yield. Wild versions were often bitter and sometimes toxic. While some groups consumed nuts like mongongo or acorns, they did so seasonally and only after elaborate detoxification steps like soaking or leaching. They were never daily staples, and they certainly weren’t the PUFA-laden snacks that line modern supermarket shelves. To imagine the Hadza walking around with almond milk lattes is pure fantasy.
The Real Building Blocks of the Human Diet
So if not grains and nuts, what did hunter-gatherers rely on? Ethnographic evidence, especially from the Hadza of Tanzania, paints a very different picture. Their diet revolves around five food categories: honey, fruit, tubers, baobab, and meat. Of these, honey and tubers are particularly central. Honey is the single most prized food of the Hadza, sometimes making up 15–20 percent of total calories. Men will climb dangerous heights to raid hives, bringing back combs dripping with sugar and bee larvae. Tubers, on the other hand, are the fallback food—the reliable starch that sustains the group through lean seasons.
Fruit and berries round out their plant staples. These wild fruits are not the oversized candy bombs you find in today’s grocery stores; they are smaller, denser, and typically higher in protein and minerals. Baobab fruit pulp and seeds provide important minerals, with the seeds being one of the few significant fat sources in the Hadza diet. Meat does play a role, but it is irregular and opportunistic—sometimes abundant, sometimes absent for days. And even when consumed, much of the meat is lean.
Taken together, the Hadza diet is overwhelmingly carbohydrate-based, with roughly two-thirds of energy coming from starches and sugars, around 15–20 percent from protein, and only about 10–15 percent from fat. This matches estimates from other indigenous groups like the Kitavans of Papua New Guinea, whose diet is nearly 70 percent carbohydrates from tubers and fruit, with very little fat. It’s also strikingly similar to the Okinawan diet—85 percent carbohydrate, mostly from sweet potatoes—which produced some of the longest-lived people on earth.
Humans Are Carbohydrate-Burning Primates
The deeper reason for this macronutrient pattern is evolutionary. Humans are primates, and primates are frugivores. In the wild, fruits make up the bulk of the diet for many monkeys and apes. Studies of wild fruit composition show that they are low in fat—on the order of just five percent by dry weight—while being rich in carbohydrates and fiber. Even chimpanzees, our closest relatives, consume meat in tiny amounts, often less than two percent of total calories. Our digestive systems, teeth, and metabolism all reflect this frugivorous heritage.
In fact, what sets humans apart is not that we abandoned fruit and starches, but that we learned to cook tubers and roots, unlocking massive amounts of digestible carbohydrate. Richard Wrangham, the primatologist who pioneered the “cooking hypothesis,” has shown that the ability to process starches with heat may have been the critical turning point in human brain evolution. Carbs, not fat, powered the expansion of our energy-hungry brains.
The Danger of the “Swampland” Diet
If ancestral diets were so carb-heavy, how did fat become glorified in the modern paleo and keto movements? The confusion stems from conflating occasional fat-rich foods (like baobab seeds or fatty game meat) with the foundation of the diet. In truth, most hunter-gatherers consumed fat sparingly. When you look across cultures—from the Hadza to the Kitavans to the Okinawans—fat intake hovers around 10 to 20 percent of calories, rarely more.
Contrast this with the modern American diet, which is roughly 40 percent fat—half of it from industrial seed oils that were never part of our evolutionary environment. When fat is layered on top of abundant carbs, you get the “metabolic swampland”: a dangerous mix that drives insulin resistance, obesity, and chronic disease. Our ancestors never lived in this swampland. Their diets were either carb-based and low in fat, or in rare cases, fat-based and seasonal (such as Inuit relying on blubber during certain times of the year). But never both at once, and never with seed oils.
Carbs as Metabolic Medicine
The implications for modern health are profound. Carbohydrates are not the enemy—they are essential for thyroid function, sex hormone balance, and metabolic rate. The conversion of T4 to active T3, the hormone that sets metabolic speed, depends on glucose availability. Progesterone production also requires adequate carbohydrate supply, which is why carb restriction often disrupts menstrual cycles. Even body temperature, a reliable marker of metabolic health, drops when carbs are insufficient.
This explains why people transitioning to pro-metabolic, high-carb, low-fat diets often feel warmer, more energetic, and hormonally balanced. It also explains why groups like the Hadza, Kitavans, and Okinawans remain lean and free of chronic disease despite consuming far more sugar and starch than the average American dares to imagine. The difference is not the presence of carbs but the absence of excessive fat, especially polyunsaturated fat.
Rethinking “Paleo”
So what did hunter-gatherers really eat? They ate honey, fruit, roots, lean meat, and the occasional fatty seed or animal organ. They did not eat large quantities of grains, nuts, or dairy. They did not eat seed oils, processed foods, or butter-drenched ribeyes. Most importantly, they did not eat high-fat, high-carb hybrid diets that suffocate the metabolism.
Our true ancestral blueprint is high-carb, moderate-protein, and low-fat. It is the diet of primates, the diet of the Hadza, the diet of the Kitavans and Okinawans, and the diet that keeps the thyroid and metabolism humming. Carbs are not just safe—they are essential. And the sooner we stop fearing sugar and start respecting the frugivorous design of our species, the sooner we can reclaim the metabolic resilience our ancestors enjoyed.
References
https://pubmed.ncbi.nlm.nih.gov/19350623/
https://anthropology.ucsd.edu/_files/Faculty%20Files/schoeninger-publications/Murray%20etal.2001.pdf
https://sciencebasedmedicine.org/what-can-we-learn-from-the-kitavans/
https://stanmed.stanford.edu/hunter-gatherer-diets-offer-clues-to-gut-bug-diversity
🌙 Bedtime Vanilla Maple Collagen Milk
🧋Sweet Sleep in a Cup
A mineral-rich, blood sugar–stabilizing nightcap to support deep, restful sleep.
If you're waking up at 2 a.m. or feeling wired at bedtime even though you're exhausted, it might be a blood sugar problem—not a willpower one. Your body needs fuel to stay calm and metabolically stable overnight. This bedtime milk delivers exactly that: fast-acting carbs to quiet cortisol, complete protein from collagen to support overnight repair, and a hefty dose of calcium to nudge melatonin production. It's sweet, simple, and deeply nourishing—no blood sugar crash, no middle-of-the-night wakeup. Just solid sleep.
🥛 Ingredients:
1 cup skim milk (rich in calcium and tryptophan)
2 tablespoons collagen powder
1 tablespoon maple syrup
Splash of pure vanilla extract
Dash of sea salt
🌀 Instructions:
Add all ingredients to a blender.
Blend on high for 20–30 seconds until smooth and frothy.
Pour into your favorite mug and sip warm or cold.
Optional: Gently heat on the stove after blending for an extra cozy feel—just don’t boil it.
💡 Why it works:
Calcium helps trigger melatonin release.
Maple syrup supplies a gentle glucose hit to keep blood sugar stable through the night.
Collagen provides glycine and protein to calm the nervous system and support tissue repair.
Skim milk keeps fat low while maximizing mineral and protein content—perfect for a metabolism-supportive cut or refeed.
🍂 Flavor Variations
1. 🥜 Peanut Butter Cup
Like drinking a peanut butter milkshake that puts you to sleep.
This version adds a hit of roasted peanut flavor that pairs perfectly with the vanilla and maple. Ideal for a little protein, carb, and calcium boost before bed—without the fat spike.
Add:
1 tablespoon peanut powder (like Organic PB2 or Just Great Stuff – no sugar added)
2. 🍁 Cinnamon Maple Dream
Add:
½ teaspoon ground cinnamon
Optional: pinch of nutmeg
Warm gently after blending for the ultimate bedtime hug in a mug.
3. 🍯 Honey Lavender
Replace maple syrup with:
1 tablespoon raw honey
Add:⅛ teaspoon food-grade dried lavender (or a drop of lavender extract)
Let the lavender steep in the warm milk after blending for 5 minutes, then strain. Incredibly relaxing for the nervous system.
Carbs Don’t Cause Insulin Resistance — Dietary Fat Does
Why cutting carbs doesn’t fix the root cause — and why sugar is part of the solution
Obesity, type 2 diabetes, heart disease, and even Alzheimer’s are often packaged under the umbrella of Metabolic Syndrome—a cluster of symptoms unified by one core dysfunction: insulin resistance.
Most clinicians and nutrition ideologies still charge that carbohydrates (especially sugar) are the villains and that eliminating them cures insulin resistance. That narrative is seductive but also misleading—and has likely hurt more people than helped.
From a pro-metabolic framing, insulin resistance isn’t caused by eating too many carbs. It’s caused by your body’s inability to use them properly. That’s a huge distinction—and alters the solution entirely.
Sugar (Carbohydrate) as a Healing Fuel, Not the Enemy
I want to be crystal clear: sugar is not inherently toxic when used in the right context. In fact, in many metabolic healing protocols (e.g. the Ray Peat model), sugar—including from ripe fruit, honey, and even sucrose—is considered one of the most metabolically supportive fuels. The Hadza (an existing primitive society in Tanzania) drink large amounts of honey everyday and have no diabetes.
Key roles sugar (glucose/fructose) plays:
Preferred fuel for liver, brain, and thyroid
Essential for replenishing glycogen in liver and muscle
Potent at lowering cortisol when consumed appropriately
Needed (in many models) for converting T4 → T3
Prevents chronic stress signals by reducing need for gluconeogenesis
Thus the logic: sugar doesn’t trigger insulin resistance—a broken metabolism does.
So why does sugar get blamed? Because almost everyone who suffers from insulin resistance is already operating in a state of metabolic suppression: under-eating, chronic stress, micronutrient deficiency, and chronic exposure to lipid toxins (especially PUFAs / seed oils). Sugar is judged in a body already damaged.
What Actually Drives Insulin Resistance
Here’s a refined list (with emphasis) of what I see as primary causal drivers:
PUFA / seed-oil accumulation in tissues
Seed oils (linoleic, linolenic acids) physically embed into mitochondrial membranes, disrupt electron transport, induce lipid peroxidation, and diminish glucose uptake.Excess dietary fat (especially PUFA) load
In ancestral diets, total fat was often low (~10 % of calories). In modern Western diets, fat has ballooned—often 30–40+ %, heavily from PUFAs. The excess free fatty acids interfere with insulin signaling (Randle cycle).Cortisol / catecholamine dominance
Chronic stress (psychological, environmental, or physiological) favors lipolysis, mobilizing fatty acids and impairing glucose uptake.Low thyroid / low metabolic drive
When your metabolic thermostat is turned down, you burn fewer carbs, producing stagnation in glucose utilization.Micronutrient deficiencies (Mg, K, B1, B3)
These are cofactors in glycolysis, Krebs cycle, pentose phosphate, etc. Without them, glucose metabolism bottlenecks.Undereating / substrate starvation (especially of carbs)
If you chronically restrict carbohydrate intake, you force the body into fat oxidation mode, reduce insulin signaling capacity, and further exacerbate metabolic inflexibility.Mitochondrial / oxidative damage
When mitochondria are oxidatively damaged (often via lipid peroxides from PUFAs), their ability to use glucose is crippled.
When your cells are overwhelmed with fatty acids and oxidative stress, they lose their ability to properly respond to insulin. Glucose uptake fails. Insulin levels rise. Over time, receptor resistance emerges. The solution isn’t to eliminate glucose—it’s to restore the cell’s ability to use it.
Muscle Is the Crucible of Glucose Burning (and Healing)
Skeletal muscle is usually the first tissue to lose insulin sensitivity. That matters, because muscle is the body’s primary sink for glucose disposal. If your muscles won’t take glucose, it gets shunted to adipose tissue or stays in circulation.
Low-carb, high-fat diets tend to worsen this: lower thyroid, higher cortisol, suppressed insulin sensitivity, and high intramuscular lipid deposition (IMCL) that blocks glucose flux (again, the Randle cycle).
So the more muscle you have (or improve in function), the better your capacity to burn sugar—and, ultimately, reduce insulin load.
Swampland Metabolism: What Breaks Your System
I like to think of a “healthy metabolism” as a well-running machine. But many people live in a swampy metabolic state—where nutrients stagnate, gradients flatten, signals get crossed. Swampland is when the body is inundated with large amounts of two different fuels: carbs and fat. What else causes this swamp?
PUFA infiltration in membranes
Low mitochondrial reserve
Chronic stress
Low energy flux (low fuel input, low output)
Toxin burden, inflammation, gut dysbiosis
Maladaptive hormonal loops
Once metabolism is in swamp mode, even “safe” foods get misprocessed. The trick to healing is to drain the swamp—restore mitochondrial energy pathways.
How to Actually Reverse Insulin Resistance (Not Just Mask It)
If insulin resistance is a wound, sugar is a tool, not a weapon. The healing process requires:
Adequate caloric intake
Chronic undereating suppresses thyroid, lowers metabolic rate, and elevates cortisol. Many people reversing metabolism—especially women—require 2,000–2,500+ kcal/day (or more, individual) with 50–60 % carbs (or more) during rehabilitation.Low fat, at least during healing
This doesn’t mean zero fat, but keep fat modest while reconditioning insulin sensitivity. For many, fat levels are capped at ~10–15 % of total calories. Focus on saturated fats (coconut oil, dairy fat, butter) in moderated amounts.Pro-metabolic carbohydrates
Favor easy-to-digest carbs: ripe fruit, fruit juice + protein, honey, root vegetables, dairy sugars. Avoid combining high fat + high sugar in the rehealing phase.Target muscle load & movement
Resistive training 2× weekly, combined with daily walking (8–10k steps), primes glucose uptake machinery (i.e. GLUT4). Over time, the more active your tissues, the more carb capacity you regain.Sunlight / circadian support
Morning sun, proper light exposure, regulated sleep help regulate thyroid, cortisol, and mitochondrial signaling.Restorative sleep & cortisol modulation
Use gentle carb + protein bedtime snacks to lower overnight cortisol surges (e.g. warm milk + honey, cottage cheese + jam).Micronutrient support
Ensure adequate magnesium, potassium, sodium, thiamine (B1), niacinamide (B3), etc. In cases of chronic depletion, short-term supplementation may be warranted.PUFA detox / fatty burden reduction
Over time, reduce dietary PUFAs, seed oils, and encourage cycles (fasting, liver support) that help mobilize and clear stored lipid toxins.Avoiding high-fat, re-feeding spikes too early
Be cautious: reintroducing large amounts of fat while metabolism is still fragile often backfires—pulling the system back into swamp mode.
Over time, insulin sensitivity recovers, glucose becomes a safe and useful fuel again, and you start to reclaim metabolic flexibility.
What About Fructose, Fatty Liver, and The “Fat + Sugar” Myth?
Fructose is demonized, but context is everything. When taken in isolation or in a low-fat matrix (fruit, honey with protein), it is typically shunted into glycogen storage (in liver) rather than lipogenesis. In fact, it’s often repackaged as fuel for vital tissues (thyroid, brain, adrenals). The danger arises when fructose is consumed alongside excess dietary fat, especially PUFAs (think: soda + french fries). That mash-up drives lipogenesis and triglyceride elevation—because the liver is overloaded, and fat export pathways are saturated.
So fruit and honey aren’t the enemy—they become part of the repair toolkit, especially when the metabolic swamp is drained.
Final Takeaway
Insulin resistance is not a carbohydrate problem - it’s a metabolic dysfunction problem. Carbs (and sugars) are not the root of the disease—they’re tools for recovery when wielded strategically.
Healing insulin resistance demands reclaiming metabolic capacity - not by fear, but by fuel, flow, and function. Eat enough. Choose carb-forward, low-fat meals. Move your muscles. Fix your sleep, hormones, and mitochondria. Ditch the fear. Heal the terrain.
Once metabolism is healed, you’ll thrive.
References
Sommerfeld, D. et al. Modern Perspective of the Rice Diet for Hypertension and Metabolic Diseases — Historical and clinical overview of Kempner’s Rice Diet and its metabolic impact.
“The Rice Diet and Duke University.” North Carolina Department of Natural and Cultural Resources — Background on Kempner’s work and the Rice Diet’s outcomes.
Kempner, W. Treatment of Massive Obesity With Rice/Reduction Diet Program. JAMA Internal Medicine (1975) — Clinical data on weight loss and insulin normalization using a low-fat, high-carb rice diet.
Scientific Publications of Walter Kempner, M.D. Vol. 2 — Duke University Archives (PDF) — Comprehensive collection of Kempner’s original studies.
“Can the Rice Diet Reverse Type 2 Diabetes?” NutritionFacts.org — Modern review of Kempner’s diet and glucose metabolism outcomes.
Minger, D. “The New USDA Dietary Guidelines: What the USDA Forgot to Mention.” Raw Food SOS (2011) — Denise Minger’s critique of mainstream nutrition science and misinterpretation of carbs vs. fats.
Minger, D. “Industrial Seed Oils: A Hidden Metabolic Disaster.” Raw Food SOS — Discussion of PUFA oxidation, mitochondrial dysfunction, and insulin resistance.
Mercola, J. “Why You Should Limit Unhealthy Fats, Not Healthy Carbs.” Mercola.com (2023) — Overview of emerging evidence connecting excess fat intake with insulin resistance.
“Insulin Sensitivity and Dietary Fat.” Mastering Diabetes — Mechanistic breakdown of how fat intake modulates insulin response in muscle and liver tissue.
“Seed Oil Misinformation.” Wikipedia — Summary of the public debate on PUFA safety, included for balanced context.
90% of Americans Are Undereating—And Reverse Dieting Is the Metabolic Fix
Learn to eat like your grandparents ate, and heal your body.
Undereating Is Silently Destroying Metabolism, Hormones, Digestion, and Mood—This Is the Strategy to Reverse It.
Reverse dieting isn’t just for bodybuilders coming off a cut or athletes trying to restore energy. It’s the unifying strategy that connects eating disorder recovery, RED-S (Relative Energy Deficiency in Sport), and the slow metabolism that plagues most of the population after years of under-eating. That includes not only classic calorie restriction but also extreme restriction of entire macronutrients. Low-carb, keto, and carnivore diets may seem therapeutic at first, but they often function as socially acceptable eating disorders. These diets can lead to significant energy deficits, hormonal suppression, and impaired metabolic function—especially when combined with intense exercise.
Whether you're coming from years of low-calorie dieting, a history of anorexia or orthorexia, or even just a hard training background with insufficient fuel, the root issue is the same: a low energy availability state (LEA).
What We Used to Eat
Our grandparents didn't count macros—they just ate real food, and plenty of it. A typical day started with a huge farm breakfast: bacon, eggs, toast with butter and jam, fried potatoes, milk or juice, and often pancakes or oatmeal on the side. Then came a massive midday lunch with meat, mashed potatoes, buttered vegetables, and dessert—often pie or cake. Dinner wasn’t light either—think steak and potatoes, more bread and butter, a second slice of pie, and a glass of milk or sweet tea. People regularly drank carbohydrates in the form of milk, juice, lemonade, or sweet tea.
Compare that to today, where many people barely pick at a salad, sip coffee for breakfast, or fast until noon. We’ve normalized starvation while wondering why we’re anxious, constipated, freezing cold, infertile, or gaining weight on what used to be considered a starvation diet.
Here’s what’s even more shocking: this modern crisis of under-eating is brand new in human history. Our hunter-gatherer ancestors—including the Hadza tribe today—consumed roughly 2,500–3,000 calories per day for women, and 3,500–5,000 for men. Even just a few generations ago, in the 1940s and 50s, women averaged around 2,500 calories and men consumed between 4,000–8,000 depending on their jobs and manual labor. This wasn’t abnormal—it was necessary for survival, metabolic repair, reproduction, and resilience. And their bodies were leaner and more functional than ours.
What Went Wrong
Another massive factor? Fat. In the 1980s, Big Tobacco bought up most of the major food companies. Around the same time, the official definition of a "low-fat" diet quietly shifted—from 10% (as seen in primitive diets) to 30%. This change skewed decades of research. Our ancestors and traditional cultures like the Hadza often consumed as little as 10-15% of calories from fat, mostly from whole-food sources like lean meat, coconuts, and milk. Today, the average American diet is around 40% fat—and a shocking 20% of total calories now come from industrial seed oils, which were originally designed as machinery lubricants, not food.
Humans are not fat-burning animals. We are primates. And like most primates, we’re built to burn carbohydrates—especially fruit and roots—as our primary fuel source. We’ve done so for nearly 7 million years. Feeding our bodies a high-fat, low-carb, seed-oil-heavy diet is a radical, modern experiment. The result? A dramatic slowing of metabolism, widespread thyroid dysfunction, and rising rates of chronic illness.
So what changed? Seed oils entered the food supply. As we began storing more fat from damaged oils and losing our ability to metabolize properly, diet culture stepped in—telling us to restrict calories to lose weight. All it did was suppress our thyroid, lower our body temperature, and increase rates of chronic disease.
The average American body today doesn’t run at 98.6°F anymore. Most hover around 96.5–97.5°F. But here’s the kicker: every degree of temperature equals about 1,000 calories burned per day. So when our intake dropped from 2,500 to 1,500, our body dropped its temperature to match, assuming a famine had arrived. This is still the same hunter-gatherer body trying to survive. We became colder, sicker, and more metabolically fragile.
Even during the Minnesota Starvation Experiment in the 1940s—conducted at the University of Minnesota—women weighed an average of 120 pounds and ate over 2,500 calories. Men consumed 4,000–8,000 per day depending on their workload. Today, we call 1,800 calories “normal,” and people wonder why they feel terrible.
Before we go further, here’s a quick scan-and-go checklist to see if you might be one of the 90%:
Undereating Red Flags
You feel cold often (especially hands, feet, nose)
Waking temp <97.8°F, pulse <75 bpm
Bloating, constipation, or slow digestion
Dry skin, thinning hair, brittle nails
Irregular or missing periods
Sleep issues, especially early waking or light sleep
Anxiety, depression, or mood swings
Constant fatigue, no matter how much you sleep
Trouble building muscle or recovering from workouts
Low libido or hormonal symptoms
Frequent fungal, bacterial, or viral infections
Puffiness, sagging skin, or changes to facial shape
If even a few of these sound familiar, your metabolism may be downregulated—and reverse dieting could be the fix.
What most people don’t realize is that under-eating is one of the most pervasive and damaging health habits in modern society. It’s not just fatigue or a missing period—chronic low energy availability is behind the explosion in autoimmune diseases, insulin resistance, gut issues, infertility, insomnia, anxiety, and even facial changes like puffiness, skin sagging, and premature aging. When your body lacks fuel, it prioritizes survival over function: it shuts down digestion, slows thyroid output, impairs detoxification, and weakens immune defense. This creates the perfect storm for fungal and bacterial infections, food intolerances, hormonal imbalance, poor motility, and systemic inflammation. It also reduces stomach acid, bile flow, and enzyme output—leading to SIBO, fungal overgrowth, histamine reactions, and poor absorption of nutrients.
Long-term undereating is also one of the most overlooked root causes of mental health disorders. The brain, liver, and nervous system require high levels of glucose to function properly, and without it, mood, memory, and resilience all decline. This is why so many people report anxiety, depression, or burnout after months or years of keto or intermittent fasting. Low energy means low serotonin, low dopamine, low progesterone, low thyroid—and zero metabolic safety. If you’re not eating enough, your body knows it, and it responds accordingly: by breaking down.
What Is Energy Availability (EA)?
Energy Availability (EA) refers to the amount of energy left over for your body to run basic biological functions after exercise is accounted for. Your thyroid, fertility, digestion, brain, and immune system all depend on this leftover energy to function. When EA is too low, your body begins downregulating non-essential functions to conserve energy—leading to symptoms like cold intolerance, missed periods, fatigue, hair loss, and muscle loss.
For the numbers people: EA = (Total Calories – Exercise Calories) ÷ Lean Body Mass (kg)
<30 cal/kg EA = Low Energy Availability (LEA)
<20 cal/kg EA = Clinical starvation
~45 cal/kg EA = Minimum for hormonal/metabolic repair
50–55 cal/kg EA = Ideal for long-term health and performance
Translation: If you’re eating under 2,000 calories as a woman or 2,500–3,000 as a man, and you exercise at all, you might be operating with too little leftover energy—even if your weight is stable.
Who Needs Reverse Dieting?
Reverse dieting is the structured way to eat more without gaining excessive fat. It’s essential for anyone who’s been under-eating, whether intentionally or accidentally. If you’ve been dieting, fasting, or doing low-carb for too long, this is your path out.
You likely need a reverse if:
You’re under-eating (<2,000 for women, <2,500–3,000 for men)
You’re not building muscle or recovering from workouts
Your libido is low, your skin is dry, or your cycle is irregular
You feel cold, anxious, moody, or fatigued
You’ve followed keto, carnivore, fasting, or other restrictive protocols
If you like numbers: Under 45 cal/kg EA = metabolic stress, even if you're overweight. It’s not about your weight—it’s about how much energy your tissues get.
The 100-Calorie Rule: How to Reverse Safely
You can’t just jump from 1,500 to 2,500 overnight. Reverse dieting adds fuel slowly so your metabolism can speed up without triggering fat gain or digestive stress.
Start slow. Add 100 calories per week until you reach the minimum threshold of 43 cal/kg. After that, slow it down to 50-calorie increases until you reach 50–55 cal/kg for long-term health.
For example: 150 lbs, 30% body fat = 47.7 kg LBM
Minimum target: 47.7 x 43 = 2,051 kcal
Ideal target: 47.7 x 50 = 2,385 kcal
Simple version: If you’re a woman, aim to build up to 2,200–2,400+ kcal. Men: 2,800–3,200+. Take your time.
Macronutrient Priorities: Carbs and Protein First
When reverse dieting, what you eat matters just as much as how much. Most people need to drastically increase carbs and protein, while keeping fat low—especially if they’re coming from a high-fat, low-carb history.
Carbohydrates are essential for liver glycogen, thyroid conversion (T4 to T3), and leptin signaling. Protein supports tissue repair and lean mass preservation. Too much fat too soon can impair insulin sensitivity and stall metabolic recovery.
Macro guideline:
Carbs: 55–65% of intake
Protein: 2.0–2.2g/kg LBM
Fat: 10–15% of calories (30–40g/day)
Simple version: Eat more fruit, juice, tubers, dairy, and lean protein. Go easy on fats until you’ve restored metabolism.
Metabolism Metrics: Temperature and Pulse
You don’t need a lab test to track metabolic recovery. Two vital signs tell the story:
Waking body temperature: should be ≥97.8°F, ideally >98.0°F, and should reach around 98.6°F later in the day
Resting pulse: 75–85 bpm (higher is better here)
Low temps and low pulse = low T3 and slowed metabolism. These markers often improve before body composition does. They’re your green light that the plan is working.
Not a tracker? You should feel warmer, more relaxed, more energetic, and more resilient. That’s healing.
Athletes and Lifters: Muscle Doesn’t Grow in LEA
Trying to build muscle while under-eating is like trying to build a house without bricks. RED-S (Relative Energy Deficiency in Sport) is the name for what happens when athletes train hard but don’t eat enough. It’s not just a female athlete problem.
Symptoms include:
Plateaued lifts
Loss of motivation
Poor recovery and disrupted sleep
Injury or persistent soreness
To grow:
Maintain at least 45 cal/kg EA
Target 50–55 cal/kg EA for bulking phases
Simple version: Eat more than you think you need. Your performance will tell you when it’s working.
Eating Disorder Recovery: Refeeding = Restoration
In ED recovery, eating more isn’t just about weight gain. It’s about repairing the thyroid, restoring brain function, rebalancing hormones, and calming the nervous system. Recovery requires far more food than most people realize.
Most women need 2,500–3,000+ calories per day to fully heal. Using the EA model ensures you’re actually supporting your body instead of just gaining weight without true restoration.
Targets:
45–55 cal/kg EA
Minimum of 2,500 kcal/day for most
Simple version: You won’t fully heal unless you consistently eat enough. Full stop.
Timeline: How Long Does It Take?
There is no one-size-fits-all timeline. Some people reach the 43 cal/kg minimum in a month; others take longer depending on their digestive capacity, fear of weight gain, or metabolic symptoms. Refeeding tends to move quickly up to around 45–48 cal/kg, then slows down as the body adapts. It may take several months—or even a year—for someone to safely reach 50–55 cal/kg.
The goal isn’t to temporarily raise your intake, but to rebuild your baseline. This is your new maintenance, not something you "hold" and then drop. Once your body has recovered, you may strategically enter short cutting phases. But for most of your life, this is where your calories should live.
A general roadmap:
Begin by adding 100 kcal/week until you reach 43 cal/kg EA (which may take 4–8+ weeks)
After that, add 25–50 kcal/week until you approach 50–55 cal/kg EA (may take months)
Stay nourished consistently, without dropping below the 43–45 cal/kg threshold unless doing a short, strategic cut
You are only ready to attempt a fat loss phase when:
Temps are ≥98.0°F
Pulse is ≥75 bpm
Digestion, sleep, and mood are solid
No binge urges or extreme fatigue
Not a planner? Keep eating more until you feel alive again. That’s when healing locks in.
Summary: The Goldilocks Zone
If you’re cold, tired, wired, not sleeping, or not progressing in the gym, you’re likely in low energy availability. This applies no matter your weight.
Quick recap:
43–48 cal/kg = recovery zone
50–55 cal/kg = performance zone
<45 cal/kg = metabolic stress
10–15% fat = best starting point for most
Bottom line: If you want a thriving metabolism, you have to feed it. Consistently. Intentionally. Slowly.
Need help calculating your EA, macros, planning your reverse, or planning for a fat-loss phase? Work with a nutritionist who understands the science, the numbers, and the real-life struggles of eating enough to heal. I’ve lived it, tracked it, and coached dozens through it. Let’s build your body back—stronger than ever.
🍓 Gluten-Free Rhubarb Crisp
There’s something deeply nostalgic about a warm fruit crisp—especially when it’s tart, tangy rhubarb bubbling beneath a golden, buttery crumble. But most recipes are loaded with flour, sugar, and heavy fats that weigh you down instead of lifting you up. This version keeps it simple and light, using just a few nourishing ingredients: sprouted oats, rice flour, honey, and a touch of butter. It’s gluten-free, low-fat, and easy to digest—perfect for a spring or summer treat that won’t derail your metabolic goals. Whether you're deep in a refeed, easing out of a cut, or just craving something sweet without the junk, this crisp delivers comfort and function in every bite.
🌾 Ingredients:
Filling:
4 cups chopped rhubarb (fresh or frozen)
2–3 tbsp honey (adjust to sweetness preference)
1 tbsp rice flour (to thicken)
Optional: pinch of salt, ½ tsp vanilla, or a splash of orange juice for brightness
Topping:
¾ cup sprouted rolled oats
¼ cup rice flour
1–2 tbsp honey (depending on desired sweetness)
1–2 tbsp butter (keep it low-fat; can use 1 tbsp if needed)
Pinch of salt
🧑🍳 Instructions:
Preheat oven to 350°F (175°C).
In a bowl, toss the chopped rhubarb with honey and rice flour. Pour into a small 8x8 baking dish.
In another bowl, mix sprouted oats, rice flour, honey, and a small amount of melted butter. Use a fork to combine until crumbly.
Sprinkle the topping over the rhubarb.
Bake for 35–40 minutes, or until the topping is golden and the fruit is bubbly.
Let cool slightly before serving. Optional: serve with a spoonful of low-fat yogurt or skim milk on the side.
🍯 Macros (Per Serving, assuming 6 servings with 1 tbsp butter total):
Calories: ~140–160
Carbs: ~28g
Fat: ~3–4g
Protein: ~2g
The Fungus Among Us
The Root Cause Doctors Rarely Acknowledge
Let me say this upfront: I had one of the worst systemic fungal and bacterial infections I’ve ever seen in a human body—and it was my own.
It started slowly. I had been keto for a couple years—thinking I was being “healthy.” But instead of feeling better, I started gaining weight. My digestion fell apart. I developed SIBO, constant bloating, and food intolerances. Looking back, I believe the low-carb, low-fiber, high-fat keto diet damaged my microbiome and starved my good gut flora, opening the door for overgrowth.
Then I "threw out my back." That’s what the ER told me, anyway. But the pain didn’t behave like a pulled muscle—it kept getting worse. Eventually, I discovered the truth: I had a bacterial infection in my spine, presenting as bulging discs and severe nerve pain. I was inflamed from head to toe.
From there, things spiraled.
I had chronic sinus and ear infections, alternating constipation and diarrhea, depression, anxiety, fatigue, and was down to only a handful of foods I could tolerate. But the worst of it came when I was breastfeeding. My daughter developed the worst thrush I’ve ever seen—her mouth looked like it was coated in cauliflower. My nipples were cracked, burning, and so painful I would scream into a pillow during feeds. But I refused to stop. I refused to give up. And I refused to switch to formula.
Instead, I spent months deep in research. Eventually, I cracked the code.
I figured out how to kill the fungus—without drugs. And once I healed myself, I knew I had to help others do the same.
Moldy Homes, Antibiotics, and Roundup: The Silent Triggers
Most people have no idea that mold exposure is almost guaranteed. Whether it’s a past leak, water damage behind the walls, or humidity buildup in the bathroom—mold spores and mycotoxins are everywhere, and once inhaled, they settle deep in your tissues.
Now stack that on top of multiple rounds of antibiotics—often prescribed for sinus infections, acne, or post-partum UTIs. These kill bacteria but leave fungus untouched, giving it free rein to overgrow.
And let’s not forget the glyphosate in our food supply—sprayed on non-organic wheat, oats, beans, and even many fruits and vegetables. Glyphosate wipes out beneficial gut bacteria and further weakens the terrain. Fungus loves the modern American body. We’re practically built to host it.
The Truth: Doctors Aren’t Trained for This
Here’s the hard truth: conventional medicine doesn’t recognize fungal overgrowth as a real diagnosis—let alone a systemic issue.
If you show up with fatigue, bloat, or brain fog, you might be offered an antidepressant. If you mention a recurring yeast infection, they’ll throw nystatin or Diflucan at it and call it a day. That’s the extent of their toolbox.
But those tools don’t work anymore. In the 70s, one Diflucan pill could knock out a yeast infection. I was once put on four a day for a month—and it did absolutely nothing. The fungus was resistant. And no one thought to ask why I wasn’t responding.
No one tested me for mold. No one mentioned the spine infection might be part of something bigger. No one ever considered that the entire terrain of my body was compromised—and fungus was running the show.
Why Herbs Work When Drugs Don’t
Once I realized the medical system had no answers, I turned to plants. And that’s when everything started to change.
Herbs work differently than pharmaceuticals. They’re complex, multi-layered, and synergistic. Fungus can’t mutate fast enough to outsmart an entire plant.
When I used herbs like grapefruit seed extract, berberine, garlic (allicin), oregano oil, caprylic acid, pau d’arco, and black walnut, I finally began to see results. The bloat started to recede. My energy returned. My daughter’s thrush began to clear. And for the first time in years, I felt like myself again.
Herbs didn’t just kill the fungus—they also helped with parasites, bacterial overgrowth, biofilm breakdown, and detox support. They worked with my body, not against it.
Die-Off Is Real (And You Shouldn’t Try This Alone)
Let me be honest: healing was not linear. When you start killing off fungal colonies, they release a storm of toxins—acetaldehyde, ammonia, mycotoxins—that overwhelm your liver, brain, and nervous system.
I went too fast in the beginning. I didn’t use binders. I didn’t support drainage. The die-off made me feel worse than before. That’s when I realized: this isn’t just about taking herbs—it’s about having a strategy.
Now, I guide others through this with support for detox pathways, liver drainage, lymphatic flow, and pacing—so the body can clear the debris without crashing.
Most Sinus Infections Aren’t Bacterial—They’re Fungal
Here’s a truth that could save you years of frustration: chronic sinus infections are almost always fungal in origin.
Doctors assume it’s bacterial, prescribe antibiotics, and send you on your way. But the relief is temporary—because they never address the fungal root. Fungus stays behind, forming colonies in the sinuses and middle ear, reactivating every time your immune system dips.
You’re not broken.
You’re just treating the wrong organism.
You Don’t Have to Do This Alone
I get it—I tried to DIY my healing, too. I read every blog, ordered every supplement, and still ended up flat on my back, bloated and brain-fogged, crying with pain during breastfeeding.
But once I had a real protocol—a functional, herbal, root-cause roadmap—everything changed.
And now I offer that roadmap to others.
Because you shouldn’t have to figure this out alone. Not when the system failed you. Not when you’re exhausted. Not when your body is screaming for help.
Ready to Heal the Root?
If you’re dealing with chronic sinus issues, bloating, anxiety, weight gain, food intolerance, or that mysterious feeling that something’s deeply off—you’re probably right.
And I want to help you fix it at the root.
🥢 Vietnamese Vermicelli Salad with Grilled Chicken
Looking for a high-protein, low-fat meal that actually tastes like summer? This Vietnamese-inspired vermicelli bowl hits every note: cool rice noodles, crisp herbs, pickled veggies, and juicy grilled chicken — all brought to life with a tangy, umami-packed dipping sauce. Unlike restaurant versions that sneak in seed oils or deep-fried shallots, this version is clean, lean, and 100% pro-metabolic. It’s also endlessly customizable: bump the carbs for a refeed, or keep it tight for a cut. And yes — it’s still so satisfying.
📝 Ingredients (Serves 2)
🍜 Vermicelli Base:
3 oz dry rice vermicelli noodles (about 2 loosely packed cups cooked)
8 oz chicken breast, cut into thin strips or chunks
1 tsp coconut aminos/tamari and/or fish sauce (for chicken marinade)
2 cups shredded romaine or butter lettuce
½ cup fresh cucumber, thinly sliced
¼ cup shredded or julienned carrot
Fresh herbs — mint, cilantro, Thai basil
🥣 Nuoc Cham-Inspired Sauce (Low-Fat):
3 tbsp fresh lime juice
2 tbsp fish sauce
1 tbsp coconut sugar or maple syrup
1 small garlic clove, minced
1 tbsp water
Optional: pinch of chili flakes
🔧 Optional Garnish (Choose 1 if fat allows):
1 tbsp crushed peanuts (~4g fat)
1 tsp fried shallots (~1.5g fat)
1 tbsp pickled onion (fat-free, adds tang)
🔥 Directions
Cook vermicelli noodles according to package. Rinse under cold water and drain well.
Marinate chicken in coconut aminos/tamari and fish sauce. Grill or sear in a cast-iron pan until fully cooked (no oil needed on the grill, maybe a small amount of ghee spray on the cast-iron).
Assemble salad bowls with lettuce, herbs, cucumber, carrot, and noodles.
Top with chicken, garnish with herbs and optional toppings.
Whisk nuoc cham sauce ingredients together. Drizzle over each bowl just before eating.
📊 Macros (Per Serving without garnish):
Calories: ~350
Protein: ~30g
Carbs: ~40g
Fat: ~4g
(Add ~4g fat per tbsp of peanuts or garnish as needed.)
Escaping the Swampland: How Low-Fat Diets Restore Metabolic Health
A very low-fat meal of chicken breast and roasted potatoes.
For years, the nutrition world has oscillated wildly between extremes—first vilifying fat, then idolizing it. Low-fat was once the gold standard, and then keto swooped in, promising effortless weight loss and boundless energy. But what if both sides missed something crucial?
As Denise Minger argued in her article In Defense of Low-Fat, we’ve thrown out a therapeutic tool that once delivered profound results. What if a very low-fat, high-carbohydrate diet (we're talking 10–15% of calories from fat) holds the key—not as a permanent way of eating, but as a metabolic reset? Evidence from forgotten clinical trials and powerful case studies shows that this approach can restore insulin sensitivity, reverse chronic illness, and reboot a damaged metabolism. Then, fat can be slowly reintroduced without regaining dysfunction.
Why Not Just Go Keto?
Low-carb and ketogenic diets can be effective at suppressing symptoms of metabolic dysfunction by removing carbohydrates, thereby reducing the need for insulin. But this doesn't mean the underlying issue—insulin resistance—is resolved.
In fact, long-term keto often leads to a condition known as physiological insulin resistance, where the body adapts to chronic carbohydrate deprivation by downregulating glucose uptake and storage. This is a protective, adaptive response—but it’s not without consequences. Over time, many keto followers develop signs of prediabetes, elevated fasting insulin, decreased thyroid function, and declining metabolic rate—even while continuing to restrict carbohydrates.
In other words, the damage can happen even if carbs are never reintroduced. Biomarkers may initially improve, but over time, thyroid function drops, stress hormones rise, and lipotoxicity—the accumulation of excess fat in organs and tissues—leads to chronic disease formation.
Then, when carbohydrates are reintroduced, things can get worse. Former keto dieters often experience blood sugar spikes, extreme fatigue, and rapid weight gain, even with modest carb intake. This isn’t just because they’re eating carbs again—it’s because their metabolism was never truly healed.
In contrast, low-fat, high-carb diets can retrain the body to use glucose effectively. They restore thyroid output, improve metabolic rate, and allow for metabolic flexibility.
WHY 10-15% FAT WORKS METABOLICALLY
What happens when you drop dietary fat to just 10-15% of your total calories? A lot more than you might think. This section summarizes five of the most well-established mechanisms explaining how very low-fat diets improve insulin sensitivity, metabolic rate, and overall health—even in the absence of calorie restriction or weight loss. Each mechanism is supported by peer-reviewed studies that collectively demonstrate how strategic fat reduction can rapidly restore glucose tolerance, repair thyroid function, and reduce the fat buildup in organs that drives chronic disease. These are not fringe ideas—they’re grounded in clinical evidence from both historic and modern trials.
To make this section easier to follow, each point includes a quick plain-language takeaway followed by a "Science Spotlight" for readers who want to dive deeper into the details.
1. Reduces Intramyocellular Lipids (IMCL)
Plain-language takeaway:
Cutting fat intake lowers fat droplets in muscle cells, improving insulin’s ability to help glucose enter cells.
Science Spotlight:
Total dietary fat—not just fat type—drives IMCL levels. In a 25‑day controlled feeding trial, subjects on a low-fat (≈31% energy from fat) diet had significantly lower muscle fat than on higher-fat diets (~36–38%). While the direct impact on insulin wasn't measured, this confirms that reducing dietary fat effectively lowers IMCL.
Study: St-Onge MP, et al. Am J Clin Nutr., 2007.
2. Lowers Lipotoxicity and Improves Mitochondrial Function
Plain-language takeaway:
Reducing dietary fat eases the fat burden on liver and pancreas, helping them function better—even before much weight is lost.
Science Spotlight:
In an 8‑week, 600 kcal/day liquid formula (20% fat) for people with type 2 diabetes, liver fat dropped ~70% and pancreatic fat declined significantly within a week. Insulin sensitivity and beta‑cell function were restored, supporting the “Twin Cycle” hypothesis
Study: Lim EL, et al. Diabetologia, 2011.
3. Improves Glucose Oxidation and Carb Tolerance
Plain-language takeaway:
When fat dominates, carb burning gets pushed aside. Lower fat intake lets the body efficiently use carbohydrates again.
Science Spotlight:
The Randle Cycle describes how high fat intake suppresses glucose oxidation. While we didn’t find a single big study to cite, decades of biochemical and clinical research confirm that lowering fat (and increasing carbs) shifts metabolism toward burning glucose more efficiently.
Foundational concept: Randle PJ, et al. Lancet, 1963. Also: Hue L, Taegtmeyer H. Am J Physiol, 2009.
4. Restores Thyroid Function + Reverses Adaptive Insulin Resistance
Plain-language takeaway:
High-carb, very-low-fat eating boosts active thyroid hormones (T3), improving metabolism and reversing the body’s adaptation to insulin resistance.
Science Spotlight:
Back in 1979, Danforth showed that switching to a high-carb, low-fat diet raised metabolic rate and increased thyroid hormone output—confirming early on that diet composition can “reactivate” thyroid function after low-carb suppression.
Study: Danforth E Jr., et al., 1979.
5. Reversal of Type 2 Diabetes Without Major Weight Loss
Plain-language takeaway:
You don’t have to lose huge amounts of weight to reverse diabetes. Cutting dietary fat—even while calories remain low—can restore blood sugar control in weeks.
Science Spotlight:
Lim’s 600 kcal/day formula diet—very low in fat—reversed diabetes in 11 obese patients: liver/pancreas fat fell ~30% in just 7 days, fasting glucose normalized, and beta-cell function was restored—all with only ~4% body weight loss
Study: Lim EL, et al. Diabetologia, 2011.
Low-Fat Isn’t What You Think It Is
Clinical low-fat diets that reversed disease used <10% fat, but modern “low fat” studies define it as 30% of calories—aka the swampland, a metabolic dead zone. This is Denise Minger's biggest point: we have redefined "low fat" in a way that neuters its therapeutic benefit.
She calls the middle zone a macronutrient swamp, where neither ketosis nor full-carb metabolism can happen cleanly. This is where modern Western diets live: moderate fat, moderate carb, high inflammation.
Why Fat Levels Should Shift With Your Metabolism
This approach uses phase-based fat manipulation, which mirrors what’s supported in the research. In the reset phase, fat is kept very low (~10%) to rapidly restore insulin sensitivity and reduce intramyocellular lipids and lipotoxicity. During the build phase, fat increases slightly (10–15%) to support glycogen storage and muscle growth while still maintaining insulin sensitivity. In the cut phase, fat stays low (10–12%) to accelerate fat loss without suppressing thyroid or metabolic rate. As you transition into the reverse phase, fat is slowly reintroduced (12–15%) while monitoring for signs of intolerance. Finally, in the maintenance phase, fat may rise to 15–30%, allowing for metabolic flexibility—if tolerated without compromising energy levels, digestion, or blood sugar.
How to Turn This Into a Metabolic Protocol
Here’s a strategic layout you can use for yourself or clients:
Metabolic Reset
Fat intake: 10% or less
Carbs: 70–75%, emphasis on fruit, juice, tubers, sugar
Protein: 15–20%, including collagen, dairy, lean meats
Goal: clear lipotoxicity, restore glucose oxidation, raise temps/pulse
Cut or Build (depending on body comp goals)
Fat: still 10–12% to maintain insulin sensitivity
Carbs: as high as tolerable
Protein: increased for muscle retention/building
Reverse and Maintenance
Slowly increase fat to 15–30% of calories
Monitor weight, body temp, libido, and mood
Add saturated fats first (dairy, cocoa butter), limit PUFA forever
Summary
Temporary fat reduction to 10% has been shown to reverse insulin resistance, MS, and heart disease
Fat impairs insulin signaling (via IMCLs), blocks glucose oxidation (Randle cycle), delays insulin clearance, and inflames organs like the pancreas and liver—even in healthy people
Restoring carb metabolism requires clearing IMCLs and lipotoxicity
“Low fat” = <10%, not 30% (which is the swamp zone)
Use this approach as a short-term metabolic reset, not a permanent solution
Slowly increase fat after the reset—up to 15–30% for long-term balance
The goal isn’t to stay low-fat forever. It’s to lose fat the right way—by restoring true metabolic health.
Let carbs and fat be friends again—but only after your body can handle it.
🥣Creamy Masa Porridge (Harina de Maíz)
Looking for a warm, comforting breakfast that’s gentle on the gut and fuels your metabolism? This creamy masa porridge is a modern spin on a Dominican classic—made with skim milk, brown sugar, and aromatic cinnamon, it's naturally gluten-free, easy to digest, and endlessly customizable. Think of it as your cozy, carb-loving answer to oatmeal—but smoother, simpler, and just as nostalgic.
Yields: 4 servings (~1½ cups each)
Time: Prep 5 min • Cook 8–10 min
Ingredients
1 cup masa harina (nixtamilized corn flour, like King Arthur)
6 cups skim milk
1 cup brown sugar OR 2/3 cup honey
½ tsp salt
2–3 whole cinnamon sticks or 1 teaspoon ground ceylon cinnamon
1 Tbsp vanilla extract
Optional: pinch of nutmeg, maple syrup, honey, or a pat of butter for serving
Instructions
Mix It Up
In a medium pot, whisk together masa harina, skim milk, brown sugar, salt, cinnamon sticks, and vanilla extract. Let sit for 5–10 minutes to hydrate the masa.Cook It Slowly
Turn heat to medium and stir continuously until it begins to bubble. As it thickens, reduce heat to low and keep whisking for 4–5 minutes until smooth and creamy. Add more milk if it gets too thick.Serve & Enjoy
Remove cinnamon sticks. Ladle into bowls and top with optional maple syrup drizzle, butter, or a sprinkle of nutmeg.
Flavor & Topping Ideas
Stir in a spoonful of collagen or gelatin for extra protein.
Add a splash of maple extract or orange blossom water for fun.
Top with fresh berries, caramelized bananas, or a dusting of cinnamon.
Serve with a side of fruit juice or steamed milk for a full pro-metabolic breakfast.
The Hidden Hypothyroid Cost of Low-Carb Diets
Low-carb diets promise a lot: quick weight loss, stable blood sugar, reduced cravings. And for a while, they deliver. But beneath the surface, a silent cost builds—especially for women. That cost is your thyroid.
Despite the early wins, long-term carbohydrate restriction can suppress thyroid function, reduce metabolic rate, and derail hormonal balance. The end result? A crash back to reality that often looks and feels like classic hypothyroidism.
Let’s break down what’s really happening—and how to spot it.
Why Carbs Matter for Thyroid Health
Carbohydrates play a direct role in the production and conversion of thyroid hormones:
Glucose is required for the conversion of T4 (inactive thyroid hormone) into T3 (the active, metabolism-boosting form).
Carbohydrate intake keeps liver glycogen stores full, which supports stable blood sugar and reduces cortisol output.
Without carbs, the body often elevates cortisol and adrenaline to maintain glucose levels—a state that suppresses T3 and slows metabolic function.
In short, your thyroid needs carbs to function properly. Depriving it long term is like trying to heat your house with the pilot light off.
Classic Symptoms of Low-Carb-Induced Hypothyroidism
Whether you’re keto, carnivore, or just living on meat and greens, here are the signs your metabolism may be tanking:
Cold hands and feet
Hair thinning or loss (especially in the shower or brush)
Constipation
Low body temperature (especially morning temps below 97.5°F)
Fatigue, even after a full night’s sleep
Brain fog or difficulty concentrating
Dry skin
Depression or emotional flatness
Low libido
Irregular or missing menstrual cycles
Weight gain despite low-calorie intake
These are not "normal aging." They're signs of a body running on survival mode.
Why Women Are Hit Harder
Women are particularly sensitive to drops in thyroid hormone and overall energy availability. Why?
Reproductive health depends on adequate thyroid and carbohydrate intake.
Female hormones (especially progesterone) require sufficient glucose to be produced and maintained.
The female body is wired to prioritize fertility and survival over fat loss—so when carbs drop, thyroid downshifts to conserve energy.
Many women on long-term low-carb diets experience amenorrhea (loss of periods), hypothyroid symptoms, and difficulty building or maintaining muscle mass. Some even lose their ability to tolerate carbohydrates at all—a condition known as physiological insulin resistance.
The Vicious Cycle of Carb Avoidance
Here’s the trap: low-carb lowers T3 and reduces your ability to metabolize carbs efficiently. Then, when you finally reintroduce carbs, your blood sugar spikes, you feel awful, and you assume carbs are the problem.
But they’re not. Your metabolism is just out of practice.
How to Heal: The Pro-Metabolic Alternative
The good news? You can rebuild. The key is to gently increase carbohydrate intake while supporting thyroid function and reducing stress.
Start with:
Whole fruit, root vegetables, and honey
Bone broth and gelatin for glycine and gut support
Dairy (if tolerated) for calcium and fat-soluble vitamins
Salt for adrenal support
Nutrients like magnesium, selenium, and vitamin A
Aim for consistent, balanced meals with protein, carbs, and a little fat. And track your body temperature—it’s a real-time window into thyroid health.
Bottom Line
Low-carb diets may feel like magic in the beginning, but long-term they can cost you your thyroid, your cycle, and your spark.
If you’re cold, tired, and stuck—don’t double down on restriction. Rebuild with carbs. Reignite your thyroid. And reclaim the energy your body was meant to have.
Scientific References
1. Carbs and T3 Conversion
Study: Effects of caloric and carbohydrate restriction on thyroid hormone metabolism in obese patients.
Source: The Journal of Clinical Endocrinology & Metabolism, 1982.
Link: https://doi.org/10.1210/jcem-54-2-386
Summary: Carbohydrate restriction significantly reduced serum T3, even when total calories were adequate. Low-carb diets suppressed active thyroid hormone conversion.
2. Low-Carb Increases Cortisol and Stress Hormones
Study: Cortisol is elevated during ketosis in lean and obese humans.
Source: The Journal of Clinical Endocrinology & Metabolism, 1994.
Link: https://doi.org/10.1210/jcem.79.6.7989461
Summary: Low-carb diets increase cortisol levels, likely to maintain blood glucose through gluconeogenesis in the absence of dietary carbs.
3. Physiological Insulin Resistance on Low-Carb
Study: Insulin resistance is a physiological response to reduced carbohydrate availability during ketogenic diets.
Source: Nutrition & Metabolism, 2009.
Link: https://doi.org/10.1186/1743-7075-6-2
Summary: Long-term low-carb diets can cause physiological insulin resistance, making it harder to tolerate carbs upon reintroduction.
4. Women’s Hormones, Fertility, and Carb Availability
Study: Effects of carbohydrate restriction on reproductive hormones in healthy women.
Source: American Journal of Clinical Nutrition, 2007.
Link: https://doi.org/10.1093/ajcn/85.3.779
Summary: Reduced carbohydrate intake lowered LH, estradiol, and progesterone levels, disrupting ovulatory function.
5. Thyroid and Energy Availability
Study: Low energy availability suppresses thyroid function and menstrual cycle in women.
Source: Medicine and Science in Sports and Exercise, 2000.
Link: https://doi.org/10.1097/00005768-200005000-00015
Summary: Women with chronically low energy availability had reduced T3 levels and disrupted reproductive hormones.
6. Glycogen and T3 Regulation
Study: Hepatic carbohydrate metabolism and the control of thyroid hormone metabolism.
Source: Trends in Endocrinology and Metabolism, 2000.
Summary: Liver glycogen stores are necessary for efficient T4 to T3 conversion; depleted glycogen impairs this process.
Why High-Fat and High-Carb Together Break Your Metabolism
🌀 The Metabolic Trap No One’s Talking About: How High-Fat + High-Carb Created a Modern Swampland
For decades, we’ve swung on the nutritional pendulum—from the sugar-fearing keto camp to the cereal-clinging standard American diet. Each side claims dominance. But what if neither is right—and both are part of the same metabolic trap?
In her provocative article "In Defense of Low-Fat," Denise Minger delivers a powerful insight: the real culprit behind modern metabolic disease isn’t carbs or fats alone—it’s the toxic combination of both. She describes our modern diet as:
“...the macronutrient ‘swamp land’ ... a toxic combination [of] very processed carbohydrates with industrial vegetable oils..."
That "swampland" isn’t just metaphor—it’s a metabolic dead zone. Dense with both fat and sugar, sludge-thick with excess calories, and stagnant with the confusion of dual-fuel overload, it has left millions inflamed, fatigued, and hormonally dysregulated.
🌀 The Metabolic Trap No One’s Talking About: How High-Fat + High-Carb Created a Modern Swampland
As Denise illustrates in her now-iconic diagram, the "magic" of dietary healing happens on either end of the fat spectrum—very low fat (<10% of calories) or very high fat (>65%). But in the middle, where most modern diets live, lies the metabolic danger zone. This is where processed carbs meet industrial fats, and where dysfunction takes root.
It’s worth noting that not everyone responds to this middle ground the same way. Cultures like the French, for example, often appear metabolically resilient even with a diet that includes upward of 30% of calories from fat. Why? Because their fat tends to come from traditional sources—like butter and cream—not industrial seed oils. Their diets also lack the decades of metabolic insult common in America: no childhood Pop-Tarts, no seed-oil-laced crackers in preschool, no 20-year history of low-fat processed diet foods and metabolic suppression.
In short: they aren’t broken. Americans, on the other hand, are exiting decades of metabolic damage—PUFA overload, stress, under-eating, low thyroid, and insulin resistance. We don’t tolerate the swamp nearly as well.
⚠️ Dual Fuel Disaster: The Real Root of Metabolic Breakdown
Human metabolism is designed to be flexible, but not omnivorous at the extremes. Carbohydrates and fats use distinct entry points into the mitochondria: glucose enters glycolysis and is funneled into the Krebs cycle, while fats undergo beta-oxidation before converging on the same pathway. This means the body can either be in a carb-burning mode or a fat-burning mode—but not both simultaneously without creating metabolic friction.
When both substrates are present in abundance, the cell prioritizes glucose oxidation and stalls fat oxidation. The excess fats, especially polyunsaturated and industrial oils, are stored or shuttled into ectopic fat depots like the liver and pancreas. This leads to mitochondrial overload, oxidative stress, and inflammatory signaling that disrupts insulin sensitivity and thyroid conversion.
This is why metabolic diseases like type 2 diabetes, non-alcoholic fatty liver, PCOS, and obesity often arise from diets high in both refined carbs and fat—not one or the other alone.
🥶 Keto: A Temporary Relief, Not a Long-Term Fix
Keto works in the short term by removing the metabolic conflict. With glucose absent, the body switches fully to fat-burning mode. This can temporarily relieve blood sugar swings, reduce inflammation, and support weight loss.
But long-term carb restriction triggers adaptations that come at a cost:
T3 (active thyroid hormone) decreases, slowing basal metabolic rate.
Leptin and insulin signaling decline, increasing appetite and impairing fertility.
The gut microbiome shifts, often reducing diversity and impairing motility.
The body becomes glucose-intolerant—not because carbs are bad, but because it's been forced to adapt to their absence.
Women are particularly sensitive to these stress signals due to higher progesterone requirements, lower muscle mass, and complex reproductive needs. Eventually, signs like cold extremities, hair thinning, low libido, and cycle irregularity creep in.
Keto doesn’t cure the swamp—it just relocates you to the other end of the map.
🌿 Our Ancestral Template: High-Carb, Low-Fat—and Thriving
Evolutionarily, carbohydrates were abundant in most human environments. Wild fruit, starchy tubers, honey, and seasonal plant foods formed the core of many diets. Fat—especially in large quantities—was rare. Wild animals, particularly in warm climates, carry very little body fat. Even large ruminants like elk or bison offer mostly lean meat with limited fat stores.
Anthropological evidence and metabolic logic suggest our physiology was shaped around a carbohydrate-dominant, low-fat intake pattern:
High-carb intake supports active thyroid hormone levels and thermogenesis.
It boosts serotonin and progesterone production, stabilizing mood and cycle health.
It facilitates efficient bile flow and digestive motility.
It allows for higher total calorie intake with less fat storage, due to low respiratory quotient interference.
In contrast to today’s abundance of deep-fried starches, our ancestors did not dip tubers in seed oils or chase fruit with cheese. They ate clean-burning carbs with lean protein and tiny amounts of natural fat—and thrived.
🚪 Getting Out of Swampland Mode: The Case for High-Carb, Low-Fat
Modern metabolic dysfunction is not about “too many carbs” or “too much fat.” It’s about the chronic coexistence of both in hyper-palatable, processed forms. Bagels with cream cheese, fries in soybean oil, donuts, pizza—each is a swamp trap.
The escape isn’t restriction. It’s selectivity. Choose your primary fuel and stick with it.
The pro-metabolic approach favors high-carb, low-fat eating because it restores the body’s default operating mode:
Glucose fuels the brain, liver, muscles, and reproductive tissues with precision.
Insulin works efficiently to shuttle nutrients into cells.
The liver clears estrogen and metabolizes thyroid hormones optimally.
Digestion becomes robust again, especially when fat intake is low enough to allow consistent bile turnover.
When you stop asking your body to juggle dueling fuels, it finally gets to perform.
💡 Bottom Line: Choose the Right Fuel—Not All of Them
We’ve spent decades playing metabolic whack-a-mole—vilifying carbs, then fat, then sugar, then meat. But the true villain is the swamp in the middle: high-fat, high-carb chaos with no clear energy direction.
If you want to heal your metabolism, ditch the swamp. Pick a side—and if you’re seeking long-term repair, radiant warmth, stable hormones, and metabolic flexibility, high-carb, low-fat is your best bet.
Eat like your ancestors: fresh fruit, honey, roots, squash, lean meats, gelatin, dairy, and a touch of natural fat.
This isn’t a fad. It’s human physiology done right.
Time to rise from the swamp—and run hot again. ✨
Molasses: The Forgotten Superfood with Deep Roots and Big Benefits
For something once as common as table salt, molasses has all but disappeared from modern kitchens. Yet for generations, it was a staple—used daily, valued as a rich source of minerals, and considered a blood-builder, particularly for women. In the rush to demonize “sugar,” we threw the baby out with the bathwater. Molasses isn't just sugar—it’s what's left behind when sugar is refined, and it’s arguably the most nourishing part.
It’s time to bring it back.
A Brief History of Molasses
Molasses is a byproduct of sugar cane or sugar beet processing. When cane is crushed and boiled to extract sucrose, the thick, dark syrup that remains is molasses. Unlike refined white sugar, which has been stripped of all micronutrients, molasses is rich in minerals, especially iron, magnesium, calcium, potassium, and manganese. In early American history, molasses was more common than sugar. It was a major trade item and a go-to sweetener in baking, beverages, and even remedies.
In many traditional cultures, molasses was used as a postpartum tonic, a fertility booster, and a digestive aid. Its deep mineral content made it an ideal food to restore depleted bodies—especially in times when access to animal foods was limited or iron-rich organs weren’t regularly consumed.
Why Molasses Is a Metabolic Ally
Ray Peat consistently highlighted the benefits of simple sugars—especially in the form of fruit juice, honey, and even refined white sugar—when consumed in the context of a nutrient-rich, low-PUFA diet. He viewed sugar not as a threat, but as a fuel, particularly for the liver, thyroid, and nervous system.
According to Peat, sugars like sucrose (glucose + fructose) can help regulate blood sugar, support thyroid conversion (T4 to T3), replenish liver glycogen, and blunt the stress response by lowering cortisol and adrenaline. He even preferred sugar over starch for many people, pointing out that starch feeds endotoxin-producing bacteria and often triggers more erratic insulin and serotonin spikes.
Molasses fits beautifully into this paradigm: it offers the same metabolic fuel as white sugar, but with a rich payload of minerals that help replenish what modern life depletes. It’s sugar, yes—but it’s sugar with a purpose.
Here’s what 1 tablespoon of blackstrap molasses provides:
Iron: ~3.5 mg (nearly 20% of daily needs for women)
Calcium: ~115 mg
Magnesium: ~50 mg
Potassium: ~500 mg
Manganese and copper: Small but significant amounts
That’s a mineral bomb in a single spoon.
Molasses supports:
Red blood cell production (thanks to iron, copper, B6)
Bone health and calcium metabolism (with calcium + magnesium)
Electrolyte balance (with potassium and magnesium)
Blood sugar regulation when consumed with protein or in the context of a nutrient-dense meal
Unlike white sugar, it doesn’t just spike blood glucose and leave you depleted—it can actually replete you, especially if you’re low in key minerals due to stress, overtraining, restrictive dieting, or heavy menstrual cycles.
Ways to Eat Molasses
Molasses has a rich, bittersweet flavor with deep caramel notes—think less like maple syrup and more like espresso-meets-brownie. If it’s too intense for you, start slow.
Some favorite ways to incorporate it:
In milk: Stir 1–2 tsp into warm raw or grass-fed milk (add vanilla, cinnamon, or a pinch of salt for a cozy mineral latte)
In smoothies: Blend 1 tsp into a banana or cacao-based smoothie with collagen and yogurt
In oatmeal: Use in place of brown sugar, or swirl into cooked oats with butter or coconut cream
In meat marinades or sauces: Molasses pairs beautifully with mustard, apple cider vinegar, or tamari
Off the spoon: If you're low on iron, a small spoonful with a piece of fruit or some cheese can do wonders
Best Practices and Considerations
Choose unsulfured blackstrap molasses, ideally organic. Sulfured molasses may contain preservatives that can be irritating for sensitive individuals.
For those with blood sugar issues, combine molasses with protein and fat (like full-fat yogurt or cheese) to blunt any potential glucose spike. That said, the glycemic index of molasses is much lower than that of white sugar or corn syrup.
If you're anemic, molasses can be a food-first alternative to iron supplements, especially if your stomach doesn’t tolerate iron pills. But it works best long term—not as a quick fix.
Summary
Molasses is more than an old-school sweetener—it's a forgotten mineral tonic with deep nutritional roots. Unlike refined sugar, it nourishes while it energizes, supports healthy iron levels, and replenishes minerals depleted by stress, restriction, or intense training.
If your body is craving something sweet, dark, and grounding—don’t reach for a candy bar. Try a spoonful of blackstrap molasses. Your metabolism, thyroid, and mitochondria might thank you.
Why Eating More Might Be the Best Thing You Can Do for Your Metabolism
What Is Energy Availability (EA) and Why Does It Matter?
If you’ve been cutting calories, skipping meals, or living off caffeine and willpower—but still feel tired, cold, bloated, or stuck—it’s not just you. And it’s not your fault. For decades, women have been told to eat less, move more, and avoid sugar at all costs. But modern science (and old-school common sense) tells a different story: your body needs fuel—real, consistent fuel—to thrive.
That’s where Energy Availability (EA) comes in. It’s a scientific way to describe how much energy your body has left over after exercise to run all the things that actually keep you alive: thyroid hormone production, detoxification, digestion, menstrual cycles, sleep, brain function, and immunity. When EA is too low, your body doesn’t have enough left to run those systems, so it starts downshifting—hard.
Most modern Americans—especially women—aren’t even close to meeting minimum EA. Compared to our ancestors and even our 1950s-era grandparents, we eat fewer calories, far less carbohydrate, and often fear sugar while overconsuming fat. This cultural shift, combined with chronic stress and government-endorsed low-calorie guidelines, has contributed to widespread metabolic suppression, thyroid dysfunction, fatigue, digestive issues, food sensitivities, and even chronic disease. Low Energy Availability is often the root cause—hidden beneath the surface of good intentions and “clean eating.” If you’ve ever felt like you’re “doing everything right” but still experiencing fatigue, sleep disturbances, or hormonal chaos, there’s a high chance you’re not hitting your EA.
Defining Energy Availability
Energy Availability is the amount of dietary energy left over for your body to run all its internal systems after you’ve accounted for exercise. In other words, it’s what’s left to support your thyroid, fertility, digestion, brain function, and immune system after movement is subtracted.
Scientifically, it’s defined as: EA = (Energy Intake - Exercise Energy Expenditure) / Lean Body Mass (kg)
Research suggests that a minimum of 45 kcal per kilogram of lean body mass (LBM) is required to maintain full physiological function in females. Anything under 30 kcal/kg LBM is considered Low Energy Availability (LEA), a state that induces metabolic suppression and hormonal dysfunction. (Loucks et al., 1998)
This is especially relevant for women who have dieted chronically, come from keto or intermittent fasting backgrounds, or engage in high levels of exercise.
How We Got Here: Modern Eating vs. Ancestral Fueling
Modern Americans are eating far less energy—and far less carbohydrate—than our ancestors or even our grandparents. Post-WWII nutrition advice began to shift public perception toward fear of sugar and cholesterol, promoting high-fat, low-carb eating patterns and chronic caloric restriction.
Government dietary guidelines—like the 1,200–1,600 calorie "weight loss plans" pushed on women—have normalized under-eating. These intake levels, combined with stress, blue light exposure, and stimulant overuse (coffee for breakfast, anyone?), mean most people are running on fumes.
Compare that to the 1930s–1950s, when women often ate 2,400–2,800 calories daily, relied on carbohydrates like milk, fruit, potatoes, and sourdough, and had far less metabolic disease.
What Happens When EA Is Too Low?
When you don’t eat enough to meet your energy needs, the body compensates. Hormones drop. Cortisol rises. Non-essential systems—like reproduction and digestion—get dialed down to conserve resources.
Common symptoms of LEA include:
Insomnia, especially waking at 2–4 a.m.
Low libido, infertility, or missing periods
Cold hands and feet
Anxiety or depression
Constipation and bloating
Weight loss resistance despite low intake
Weak immunity and poor wound healing
From a functional medicine perspective, low EA often underpins issues like hypothyroidism, estrogen dominance, and adrenal fatigue. You can’t out-supplement an energy deficit.
How to Calculate Your EA (and Fix It)
Estimate your Lean Body Mass (LBM): This can be measured using InBody scans, DEXA, or estimated based on body fat %.
Multiply LBM (in kg) by 45: This is your minimum intake goal in kcal/day.
Example: A woman with 50 kg LBM needs at least 2,250 kcal/day.
Add back food slowly if you’ve been under-eating: Reverse dieting is a strategic way to avoid weight gain while restoring EA.
Minimize cardio: Excess cardio drains available energy and prolongs LEA. Focus on strength training and low-intensity walking or Zone 2 movement.
Track consistently: Use tools like Cronometer to ensure you're hitting total calories. Prioritize meeting energy first, then macros.
Scientific References
Loucks, A. B., et al. (1998). Energy availability, not body fatness, regulates reproductive function in women. Exercise and Sport Sciences Reviews.
Mountjoy, M., et al. (2014). Relative Energy Deficiency in Sport (RED-S) Consensus Statement. British Journal of Sports Medicine.
Melin, A., et al. (2015). Energy availability and the female athlete triad in active women. Clinical Journal of Sport Medicine.
Final Thoughts: EA Is the Foundation
You can’t rebuild your metabolism, restore your hormones, or heal your gut if you’re operating from a place of scarcity.
Energy Availability is the bare minimum—not a luxury. And while the mainstream may still push "eat less, move more," the science is clear: under-eating doesn’t just slow weight loss, it shuts down vitality.
Start by fueling generously, tracking accurately, and honoring your body's demand for nourishment. Reaching your EA is the difference between surviving and thriving.
🛏️ Sleep Like a Metabolic Champ
Pro-Metabolic Strategies for Deep, Restorative Sleep
😴 Sleep is not a luxury. It's one of the most metabolic processes your body performs. If you're waking up at 2–3 a.m., tossing and turning, or dragging yourself through the day, your sleep setup—and your metabolism—needs an overhaul.
Here’s how to dial in sleep support using science-backed and pro-metabolic principles:
🌞 Support Your Circadian Rhythm
Get sunlight first thing in the morning—at least 10 minutes outdoors helps anchor your circadian rhythm.
Use incandescent light bulbs during the day (avoid LEDs and CFLs), which mimic natural light and support energy without damaging blue light.
No screens 1 hour before bed—phones and TVs blast your brain with cortisol-spiking blue light.
Switch to amber light bulbs or red night lights in your bedside lamp and bathroom at night.
Consider blue light-blocking glasses after sunset if screen use is unavoidable.
🌡️ Create a Sleep Sanctuary
Keep your room cool and dark—ideal temperature is 65–68°F.
Use blackout curtains, turn off or cover any blinking lights, and ban all electronics from the bedroom.
No nightlights unless they’re red/amber spectrum only (and low wattage).
🍯 Balance Your Blood Sugar for Sleep
Night wakings (especially between 2–4 a.m.) are usually a cortisol response to low glycogen.
Eat a bedtime snack with carbs, protein, and salt to keep blood sugar stable through the night (e.g., warm milk + honey + pinch of salt).
Avoid fasting or under-eating, especially if your total daily calories are below your minimum energy availability.
🧠 Calcium, Cortisol & Melatonin
Calcium is a precursor to melatonin, and many women in LEA are deficient.
Prioritize calcium-rich pro-metabolic foods: dairy, sardines, bone broth.
If needed, supplement with food-based calcium (not citrate).
If you're in low energy availability (LEA) or hypothyroid, insomnia is often your body screaming for nourishment.
💥 Low Energy = Low Sleep Quality
Chronically low food intake leads to high cortisol, low melatonin, poor thyroid function, and restless sleep.
Track your intake and make sure you're eating enough—especially carbs.
Avoid extreme low-carb or low-fat diets; both impair sleep quality.
✅ Your Pro-Metabolic Sleep Checklist
☀️ Morning sun + incandescent light during the day
🧠 Amber or red light at night
📴 No screens 1 hour before bed
🌡️ Cool, dark, tech-free bedroom
🥛 Bedtime carb + protein + salt snack
🧀 Daily calcium-rich foods
💤 Hit your calorie target to avoid LEA
Sleep isn’t just about rest—it’s a reflection of your metabolic status. Optimize it, and you’ll feel the difference in your energy, mood, and healing speed.
Sleep like your metabolism depends on it—because it does. 🌙✨